Introduction & Background of Multiple System Atrophy (MSA)
Multiple System Atrophy (MSA) is a rare, progressive, and fatal neurodegenerative disorder. It was historically known by other names, including Shy-Drager syndrome, olivopontocerebellar atrophy (OPCA), and striatonigral degeneration.
The name “Multiple System Atrophy” reflects the core of the disease: the degeneration or “atrophy” of cells in multiple areas of the brain and spinal cord. This damage affects several key “systems” that control vital involuntary bodily functions, leading to a combination of symptoms that impact movement, balance, blood pressure, and bladder control.
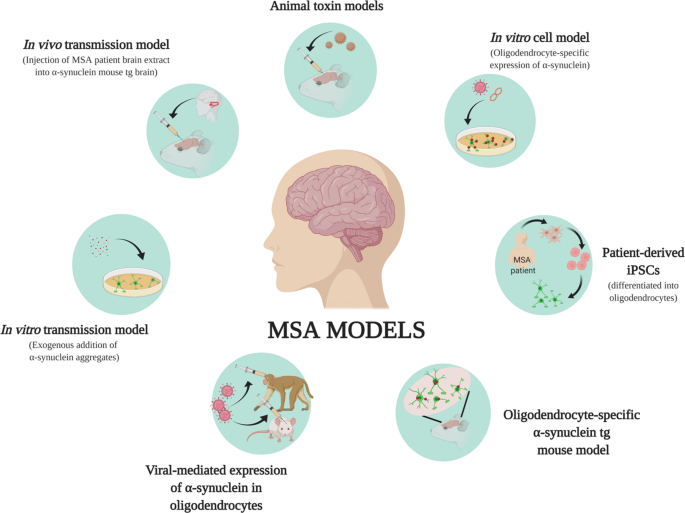
MSA is classified as a synucleinopathy, meaning it involves the abnormal accumulation of a protein called alpha-synuclein within glial cells in the brain (specifically, in oligodendrocytes, forming glial cytoplasmic inclusions or GCIs). This is the same protein that clumps in Parkinson’s disease, but in a different pattern and cell type. MSA is a sporadic condition, meaning it typically occurs at random, with no known inheritance pattern in the vast majority of cases.
Causes of Multiple System Atrophy (MSA)
The exact cause of MSA remains unknown. However, scientific research has identified key pathological processes:
- Alpha-Synuclein Accumulation: The hallmark of MSA is the buildup of the misfolded alpha-synuclein protein in the brain’s support cells (glial cells). These toxic protein clumps are thought to disrupt cellular function, lead to inflammation, and ultimately cause the death of neurons in areas controlling movement, balance, and autonomic functions.
- Sporadic Occurrence: For most patients, there is no family history of the disease, and no specific genetic or environmental trigger has been consistently identified. It is believed to result from a complex and poorly understood interaction between genetic susceptibility and unknown environmental factors.
- Risk Factors: The only well-established risk factors are age (typically onset in the 50s or 60s) and a slightly higher incidence in men compared to women.
Indications of Multiple System Atrophy (MSA)
“Indications” in a medical context often refer to reasons to suspect a disease or to use a particular treatment. For a patient, the initial indications (or warning signs) of MSA can include:
- The onset of Parkinson-like symptoms (slowness, stiffness, tremor) that do not respond well to Levodopa medication.
- A significant drop in blood pressure upon standing (orthostatic hypotension), causing dizziness or fainting.
- Urinary incontinence or a sudden, urgent need to urinate.
- Problems with coordination and balance (ataxia), such as slurred speech, unsteady gait, and clumsiness.
The diagnosis is primarily clinical, based on these indications, and may be supported by MRI scans showing specific patterns of brain atrophy.
Symptoms of Multiple System Atrophy (MSA)
MSA symptoms are broadly divided into two categories, though there is significant overlap:
1. Parkinsonian Symptoms (MSA-P subtype – most common):
- Slowness of movement (bradykinesia)
- Muscle stiffness and rigidity
- Tremors (often irregular and not the classic “pill-rolling” tremor of Parkinson’s)
- Impaired balance and posture, leading to falls
2. Cerebellar Symptoms (MSA-C subtype):
- Loss of coordination and balance (ataxia)
- Slurred, slow, or quivering speech (dysarthria)
- Difficulty swallowing (dysphagia)
- Visual disturbances, such as blurred vision and trouble focusing
3. Autonomic Dysfunction (Affects both subtypes):
- Severe orthostatic hypotension: A sharp drop in blood pressure when standing, causing lightheadedness, dizziness, and fainting.
- Urinary dysfunction: Incontinence, urgency, frequent infections, or incomplete bladder emptying.
- Sexual dysfunction: Erectile dysfunction in men and loss of libido in both sexes.
- Constipation
- Abnormal sweating and body temperature control
- Inspiratory stridor: A harsh, high-pitched sound during inhalation due to vocal cord paralysis.
Other symptoms can include rapid eye movement (REM) sleep behavior disorder (acting out dreams), chronic fatigue, and cognitive and emotional changes.
Prevention Strategies of Multiple System Atrophy (MSA)
There are currently no known ways to prevent MSA. Because its cause is unknown and it is sporadic, no lifestyle changes, diets, or medications have been proven to reduce the risk of developing the disease. Research is focused on understanding the initial triggers of alpha-synuclein misfolding to eventually develop preventive strategies.
Myths and Facts About Multiple System Atrophy (MSA)
| Myth | Fact |
|---|---|
| MSA is the same as Parkinson’s disease. | While they share some symptoms, MSA is a distinct disease with a different underlying pathology, faster progression, and poorer response to Parkinson’s medications. |
| MSA is hereditary. | In the vast majority of cases, MSA is sporadic and not passed down through families. |
| There are effective treatments to cure or stop MSA. | Currently, there is no cure for MSA. Treatments are focused on managing symptoms and improving quality of life. |
| Only older people get MSA. | While most common in the 50-60 age group, MSA can occasionally occur in younger or older adults. |
| If you have a tremor, it must be MSA or Parkinson’s. | Many conditions cause tremors. The presence of severe autonomic symptoms (like fainting) alongside parkinsonism is a key indicator of MSA. |
Treatments and Therapy
Management of MSA requires a multidisciplinary approach tailored to the individual’s symptoms.
Medication-Based Treatments
- For Parkinsonism: Levodopa may be tried, but only a minority of MSA patients experience significant or sustained benefit. Other Parkinson’s medications are less effective.
- For Low Blood Pressure: Fludrocortisone, midodrine, droxidopa, and pyridostigmine can help raise blood pressure. Salt and fluid intake is often increased.
- For High Blood Pressure when lying down: Elevating the head of the bed and sometimes medication timing adjustments are used.
- For Urinary Incontinence: Oxybutynin or tolterodine. For incomplete emptying, intermittent self-catheterization may be necessary.
Surgical Treatments
- In severe cases of inspiratory stridor, a tracheostomy may be required to maintain an open airway.
- Deep Brain Stimulation (DBS), used for Parkinson’s, is generally not effective for MSA and is not recommended.
Physical Therapy and Rehabilitation
- Crucial for maintaining mobility, strength, and flexibility.
- Helps prevent falls through balance training and the use of assistive devices (walker, wheelchair).
- Speech therapy can help with swallowing difficulties and speech problems.
Lifestyle and Behavioral Interventions
- Diet: Small, frequent, low-carbohydrate meals to minimize post-meal blood pressure drops. Increased salt and water intake.
- Compression Garments: Abdominal binders and compression stockings can help prevent blood from pooling in the legs.
- Sleep Safety: For REM sleep behavior disorder, padding the bedroom floor may be necessary.
Alternative and Complementary Medicine
- There is no evidence that alternative therapies can alter the course of MSA. Some patients may find therapies like acupuncture or massage helpful for managing specific symptoms like muscle stiffness or pain, but they should be used alongside, not instead of, standard care.
Psychotherapy and Counseling
- Essential for patients and families to cope with the emotional and psychological impact of a progressive, life-limiting diagnosis. It can help manage depression, anxiety, and grief.
Immunizations and Vaccines
- There are no vaccines to prevent or treat MSA. However, staying up-to-date with recommended vaccines (e.g., flu, pneumonia) is important to prevent secondary complications.
Stem Cell Therapy
- This is an area of active research but is still highly experimental. There are currently no proven, safe, or effective stem cell treatments for MSA. Patients should be cautious of clinics offering unproven and costly therapies.
Gene Therapy
- Like stem cell therapy, gene therapy for MSA is in the early stages of preclinical research and is not available as a treatment.
Top 20 FAQ with Answer on Multiple System Atrophy (MSA)
1. What is the life expectancy for someone with MSA?
The average life expectancy from diagnosis is between 6 to 10 years, but this varies significantly from person to person.
2. Is MSA fatal?
Yes, MSA is a progressive and fatal disorder, most commonly due to respiratory or cardiac complications.
3. Is MSA hereditary?
No, it is almost always sporadic. Family history is extremely rare.
4. What is the difference between MSA and Parkinson’s disease?
MSA progresses faster, responds poorly to Levodopa, and involves more severe autonomic failure early in the disease course.
5. Can MSA be cured?
No, there is currently no cure for MSA.
6. What treatments are available?
Treatment focuses on symptom management: medications for blood pressure, physical therapy for mobility, and interventions for bladder and speech problems.
7. Why do I faint when I stand up?
This is called orthostatic hypotension, caused by the autonomic nervous system failing to properly regulate blood pressure upon standing.
8. Will I lose my ability to walk?
As the disease progresses, mobility is typically affected, and most patients will eventually require a wheelchair.
9. Can MSA affect my thinking and memory?
While MSA is primarily a movement and autonomic disorder, some patients can develop cognitive impairment, though severe dementia is not typical.
10. What is the “P” and “C” in MSA-P and MSA-C?
MSA-P (Parkinsonian subtype) is dominated by stiffness and slowness. MSA-C (Cerebellar subtype) is dominated by coordination and balance problems.
11. How is MSA diagnosed?
There is no single test. Diagnosis is based on clinical symptoms, neurological examination, and sometimes an MRI to look for specific patterns of brain atrophy. A poor response to Levodopa is a key clue.
12. What specialist should I see?
A neurologist, preferably one specializing in movement disorders or autonomic neurology.
13. Can diet or exercise help?
A high-salt, high-fluid diet can help with low blood pressure. Physical therapy and exercise are vital for maintaining function as long as possible.
14. What is stridor?
A harsh, high-pitched sound when breathing in, caused by weakness or paralysis of the vocal cords. It is a serious symptom that requires medical attention.
15. Are there any new drugs being developed?
Yes, research is ongoing, particularly focused on drugs that can target and clear the misfolded alpha-synuclein protein.
16. How can I manage my bladder problems?
Medications can help with overactive bladder, while intermittent catheterization may be needed if the bladder doesn’t empty fully.
17. Is it safe to have surgery with MSA?
It requires careful planning with an anesthesiologist who understands the unique autonomic challenges of MSA.
18. How can I reduce my risk of falls?
Use assistive devices (walker, cane), remove tripping hazards at home, and work with a physical therapist on balance training.
19. Where can I find support?
Organizations like the Multiple System Atrophy Coalition (USA) and the Multiple System Atrophy Trust (UK) provide invaluable resources, support groups, and information for patients and caregivers.
20. What is the most important thing for a caregiver to know?
Caring for someone with MSA is challenging. Prioritize your own well-being, seek support, and focus on maximizing quality of life and comfort for your loved one.
Conclusion
Multiple System Atrophy is a devastating and complex disease that presents immense challenges for patients and their families. While the prognosis is currently poor, and a cure remains elusive, a proactive and multidisciplinary management approach can make a significant difference in quality of life. Ongoing research into the underlying mechanisms of alpha-synuclein pathology offers hope for future therapies that could slow, halt, or even reverse the progression of this relentless condition. Until then, compassionate care, robust support systems, and symptom-focused treatment are the cornerstones of managing MSA.
Find Trusted Cardiac Hospitals
Compare heart hospitals by city and services — all in one place.
Explore Hospitals
My husband has been doing the MSA-5 formula from www. limitlesshealthcenter. com for about 5 months. It doesn’t seem like he’s getting any better, but overall, he actually has. My husband says it’s done him a lot of good in terms of balance and ability to walk and get up from chairs, which has been very noticeable. He can now write without his hands shaking. He feels better now than he has felt in years, and he can feel his strength again. We feel very fortunate to have learned about the MSA-5 formula.
This guide explains Multiple System Atrophy in a very clear and structured way, especially how movement problems, autonomic symptoms, and neurological decline are connected, helping readers understand why early diagnosis and supportive care are so important. The way you described causes, clinical features, and management options gives patients and families a realistic yet hopeful perspective on living with this complex condition. A very informative and compassionate resource for anyone trying to better understand MSA.