Introduction & Background of Rasmussen’s Encephalitis
Rasmussen’s encephalitis (RE) is an extremely rare and devastating chronic neurological disorder characterized by unilateral inflammation of the brain, leading to progressive neurological and cognitive deterioration. It primarily affects one hemisphere (side) of the brain.
First described by Dr. Theodore Rasmussen in 1958, it is classified as an autoimmune encephalitis. The immune system mistakenly attacks healthy brain tissue, but unlike other autoimmune conditions, the attack is typically focused on a single cerebral hemisphere. The inflammation is persistent (“chronic”) and leads to tissue scarring (gliosis) and loss of brain cells (atrophy).
The disease most commonly begins in childhood, with an average onset age of 6, but it can also occur in adolescents and adults. Its progression and resistance to conventional anti-inflammatory treatments make it a particularly challenging condition to manage.
Causes of Rasmussen’s Encephalitis
The exact cause of Rasmussen’s encephalitis is not fully understood, but it is widely believed to be an autoimmune disorder. The leading hypothesis involves a complex interaction between a viral trigger and a genetic predisposition.
- Autoimmune Response: The body’s immune system produces antibodies (such as anti-GluR3 antibodies) and cytotoxic T-cells that attack neurons in one brain hemisphere.
- Viral Trigger: Some theories suggest a common virus, like the cytomegalovirus (CMV) or Epstein-Barr virus (EBV), may act as an initial trigger in susceptible individuals, setting off the misguided autoimmune response.
- Genetic Predisposition: While not directly hereditary, certain genetic factors may make some individuals more vulnerable to developing this type of autoimmune reaction. It is not a disease that runs in families.
Indications of Rasmussen’s Encephalitis
“Indications” in a medical context often refer to the signs that point toward a diagnosis. For RE, key indications include:
- Focal Seizures: The most prominent indication, often starting in one part of the body (e.g., a hand or foot) and potentially spreading. These seizures are frequently resistant to multiple anti-seizure medications (drug-resistant epilepsy).
- Unilateral Neurological Deficits: Weakness or paralysis on one side of the body (hemiparesis), opposite the affected brain hemisphere.
- Progressive Cognitive Decline: Loss of cognitive functions, including memory, reasoning, and speech, particularly if language-dominant hemisphere is affected.
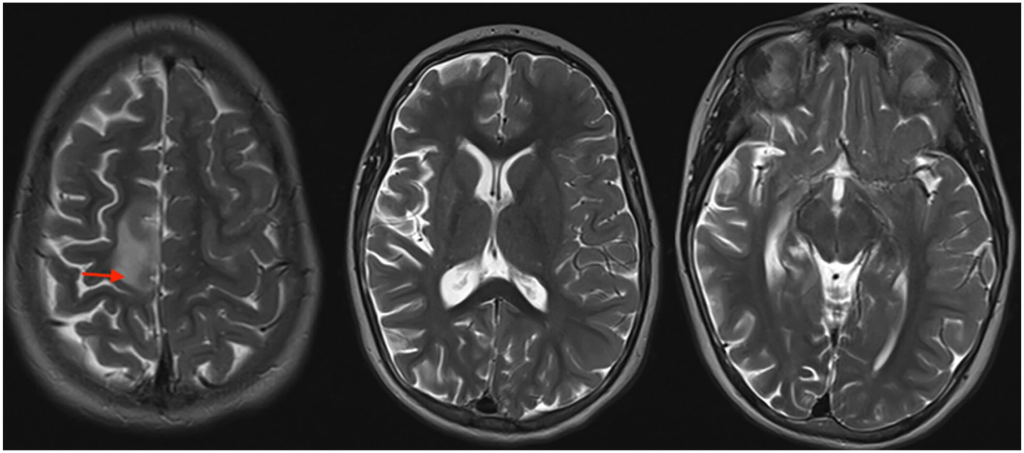
- Unilateral Brain Atrophy: MRI scans revealing shrinkage and scarring in one cerebral hemisphere, which worsens over time.
Symptoms of Rasmussen’s Encephalitis
Symptoms progress through stages, often beginning with a “prodromal” phase with infrequent seizures, followed by an “acute” phase with frequent, severe seizures and neurological decline.
- Frequent and Severe Epileptic Seizures: Often focal motor seizures (affecting one limb or side of the face) that can evolve into convulsive seizures. A specific and severe type is Epilepsia Partialis Continua (EPC)—continuous jerking of a limb or group of muscles for hours, days, or even years.
- Hemiparesis: Progressive weakness and loss of control on one side of the body.
- Cognitive Deterioration: Decline in learning, memory, and intellectual abilities.
- Speech Problems (Aphasia): If the language-dominant hemisphere (usually the left) is affected, patients may experience difficulty speaking, understanding language, or both.
- Visual Field Defects: Loss of vision on one side (homonymous hemianopia).
- Behavioral Changes: Irritability, mood swings, and personality changes.
Prevention Strategies of Rasmussen’s Encephalitis
There are currently no known prevention strategies for Rasmussen’s encephalitis. Because the cause is not definitively known and likely involves an unpredictable autoimmune response, it is not possible to prevent its onset. The focus is on early diagnosis and aggressive treatment to prevent further brain damage and control symptoms.
Myths and Facts About Rasmussen’s Encephalitis
| Myth | Fact |
|---|---|
| RE is a form of childhood cancer. | RE is not cancerous. It is an inflammatory, autoimmune disorder. |
| It is contagious. | You cannot “catch” RE from someone who has it. It is an autoimmune condition, not an infection. |
| Seizures can be controlled with medication alone. | RE is notoriously drug-resistant. Most patients require surgical intervention for seizure control. |
| Both sides of the brain are always affected. | The defining feature of RE is its unilateral (one-sided) focus, though in extremely rare cases, the other hemisphere may become involved later. |
| Patients with RE always have severe intellectual disability. | Outcomes vary. While cognitive impact is significant, especially without treatment, functional hemispherectomy can halt progression and allow for rehabilitation and improved quality of life. |
Treatments and Therapy
Treatment aims to control seizures, halt the inflammatory process, and manage neurological symptoms. A multi-modal approach is essential.
Medication-Based Treatments
- Antiseizure Medications (AEDs): Used to try and control seizures, though they are often ineffective alone. Examples include levetiracetam, clobazam, and topiramate.
- Immunotherapies: These target the underlying inflammatory process.
- Corticosteroids: (e.g., prednisone) High-dose pulses can reduce inflammation.
- Intravenous Immunoglobulin (IVIG): A blood product that modulates the immune system.
- Plasmapheresis (PLEX): A procedure to filter harmful antibodies from the blood.
- Tacrolimus/Rituximab: Other immunomodulating drugs used in some cases.
Surgical Treatments
- Functional Hemispherectomy/Hemispherotomy: This is the only curative treatment for seizures in RE. It involves disconnecting the affected hemisphere from the healthy one while leaving it in place. This stops seizure spread and halts disease progression. It is most effective when done early, but results in permanent weakness on the opposite side of the body.
Physical Therapy and Rehabilitation
Crucial for maximizing physical function after surgery or to manage hemiparesis. It helps maintain muscle strength, flexibility, and mobility.
Lifestyle and Behavioral Interventions
- Ketogenic Diet: A high-fat, low-carbohydrate diet that can help reduce seizure frequency in some drug-resistant epilepsy cases.
- Safety Modifications: Adapting the home environment to prevent injury during seizures.
- Structured Routines: Helpful for managing cognitive and behavioral challenges.
Alternative and Complementary Medicine
- CBD Oil: Some families report reduced seizure frequency or improved sleep, though robust evidence for RE is lacking.
- Stress Reduction: Techniques like mindfulness and yoga may improve overall well-being but do not treat the core disease.
Psychotherapy and Counseling
Essential for patients and families to cope with the emotional and psychological impact of a chronic, progressive illness.
Immunizations and Vaccines
There is no vaccine for RE. Standard immunizations are generally safe, but decisions should be made in consultation with a neurologist, especially during active immunotherapy.
Stem Cell Therapy
Currently experimental and not a standard treatment for RE. Research is ongoing into its potential for modulating the immune system or repairing neurological damage.
Gene Therapy
Not currently available for RE. It remains a topic of future research for many neurological disorders.
Top 20 FAQ with Answer on Rasmussen’s Encephalitis
1. What is Rasmussen’s Encephalitis?
It is a rare, chronic inflammatory neurological disease that typically affects one brain hemisphere, causing severe seizures and neurological decline.
2. Who gets RE?
It primarily affects children under 10, but adolescent and adult-onset cases are also documented.
3. Is it fatal?
With modern treatments, particularly surgery, it is not typically fatal. However, without treatment, the complications of uncontrolled seizures and neurological decline can be life-threatening.
4. Is RE hereditary?
No, there is no evidence that it is a hereditary or genetically passed-down condition.
5. What is the first sign of RE?
Usually, the first sign is the onset of focal seizures, often difficult to control with medication.
6. How is RE diagnosed?
Diagnosis is based on clinical symptoms (seizures, hemiparesis), EEG showing unilateral abnormalities, and MRI showing progressive atrophy of one hemisphere.
7. Can medications cure RE?
No, there is no pharmacological cure. Immunotherapies can slow progression, but surgery is the only intervention that can stop seizures permanently.
8. What is a functional hemispherectomy?
It is a surgical procedure that disconnects the diseased hemisphere from the healthy one, stopping seizures while leaving the brain tissue in place.
9. What are the side effects of hemispherectomy?
The main side effect is permanent weakness on the opposite side of the body (hemiparesis) and a loss of peripheral vision on that side.
10. Can a person live a normal life with one brain hemisphere?
Yes, the brain has remarkable plasticity, especially in young children. The healthy hemisphere can take over many functions, allowing for a good quality of life, though with some physical limitations.
11. Why does the brain deteriorate in RE?
The autoimmune attack causes inflammation, which kills neurons and supporting cells, leading to scarring (gliosis) and tissue loss (atrophy).
12. Is RE considered an autoimmune disease?
Yes, it is classified as an immune-mediated encephalitis.
13. Can adults get RE?
Yes, though it is much rarer. Adult-onset RE often has a slower progression than the childhood form.
14. What is Epilepsia Partialis Continua (EPC)?
It is a condition of continuous jerking in one part of the body that can last for extended periods and is a classic feature of RE.
15. Can the disease spread to the other side of the brain?
This is very rare. The disease is almost always confined to one hemisphere.
16. What is the life expectancy for someone with RE?
With successful surgical treatment, life expectancy can be near normal. The goal of treatment is to manage the condition and prevent fatal complications.
17. Are there any support groups for RE?
Yes, organizations like the Rasmussen’s Encephalitis Children’s Project and the Brain Foundation provide resources and support for families.
18. Can speech therapy help?
Yes, especially if the language hemisphere is affected. Speech therapy is critical for rehabilitation post-surgery or to maximize communication abilities.
19. What is the role of the ketogenic diet?
It is used as an adjunct therapy to help reduce seizure frequency when medications are ineffective.
20. Is there ongoing research for RE?
Yes, research focuses on better understanding the autoimmune mechanisms, improving immunotherapies, and refining surgical techniques.
Conclusion
Rasmussen’s encephalitis remains a formidable and rare neurological challenge. Its relentless, unilateral attack on the brain causes severe seizures and progressive disability. While the absence of a known cause or prevention strategy is daunting, significant progress has been made in management. The combination of immunomodulatory therapies and, most decisively, functional hemispherectomy, has transformed the prognosis for many patients. This surgical intervention, while life-altering, offers the best chance to halt disease progression and provide a path toward a stable future. Continued research into its autoimmune mechanisms holds the promise for more targeted and less invasive treatments in the years to come.
Find Trusted Cardiac Hospitals
Compare heart hospitals by city and services — all in one place.
Explore Hospitals
This guide does a great job making Rasmussen’s Encephalitis easier to understand for general readers, especially by explaining how early symptoms, seizures, and neurological changes are connected and why timely diagnosis is so important. The way you described treatment approaches and long-term care helps families realize that with proper medical support and monitoring, better management and quality of life are possible. A very informative and reassuring resource for anyone trying to understand this rare neurological condition.