Introduction & Background of Cryoglobulinemia
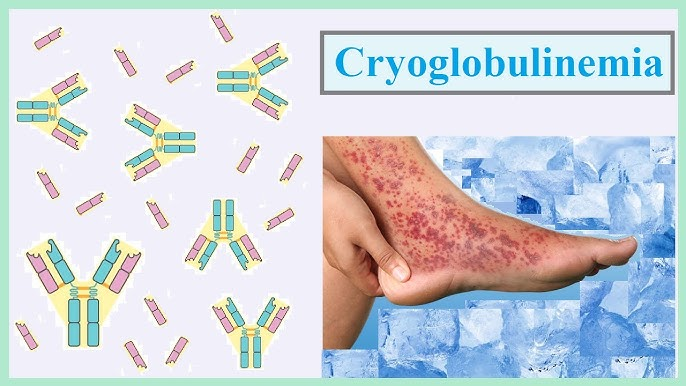
Cryoglobulinemia is a rare medical condition characterized by the presence of abnormal proteins in the blood called cryoglobulins. The name comes from the Greek words “cryo” (cold) and “globulin” (a type of protein). The defining feature of these proteins is that they clump together (precipitate) in the blood at temperatures below normal body temperature (37°C or 98.6°F) and dissolve again when warmed.
These clumps can thicken the blood and deposit in small and medium-sized blood vessels throughout the body, leading to inflammation, reduced blood flow (ischemia), and damage to tissues and organs, particularly the skin, joints, nerves, and kidneys. Cryoglobulinemia is often, but not always, linked to an underlying disease, most commonly hepatitis C infection.
Causes of Cryoglobulinemia
Cryoglobulinemia is primarily caused by the production of cryoglobulins, which are often a response to an underlying condition. It is classified into three main types based on the type of antibody involved:
- Type I: Composed of a single type of antibody (usually IgM). This type is most commonly associated with cancers of the blood or immune system, such as multiple myeloma or Waldenström’s macroglobulinemia.
- Type II & III (Mixed Cryoglobulinemia): Composed of multiple types of antibodies (typically IgM and IgG). These are most frequently linked to chronic inflammatory or infectious diseases.
- Hepatitis C virus (HCV) is the leading cause, responsible for the vast majority of mixed cryoglobulinemia cases.
- Other infections: Hepatitis B, HIV, bacterial endocarditis.
- Autoimmune diseases: Sjögren’s syndrome, systemic lupus erythematosus (SLE), rheumatoid arthritis.
- Lymphoproliferative disorders.
In many cases, an underlying cause is never found, which is referred to as Essential Cryoglobulinemia.
Indications of Cryoglobulinemia
The “indications” for suspecting cryoglobulinemia are the clinical signs and risk factors that prompt a doctor to test for it. These include:
- A patient presenting with the classic “Meltzer’s Triad” of symptoms: purpura (skin rash), joint pain, and weakness.
- Unexplained nerve damage (neuropathy) manifesting as numbness, tingling, or weakness.
- Known history of a condition strongly associated with cryoglobulinemia, especially Hepatitis C.
- Signs of kidney inflammation (glomerulonephritis), such as blood or protein in the urine.
- Unexplained skin ulcers or gangrene, particularly in the fingers and toes.
Symptoms of Cryoglobulinemia
Symptoms occur when the cryoglobulin protein clumps in the blood vessels, especially in cooler parts of the body or during cold exposure. They can vary widely but often include:
- Skin:
- Purpura: A purple-red, raised rash, most commonly on the legs.
- Raynaud’s phenomenon: Fingers and toes turning white, then blue, and then red in response to cold or stress.
- Ulcers and Gangrene: Severe cases can lead to skin breakdown and tissue death.
- Joints: Pain and aching (arthralgia), often in the hands and knees.
- Nerves: Peripheral neuropathy causing numbness, tingling, burning, or weakness, usually in the hands or feet.
- Kidneys: Damage (glomerulonephritis) leading to proteinuria, hematuria, high blood pressure, and potentially kidney failure.
- General: Fatigue, weakness, and generalized malaise.
- Other: Abdominal pain, liver involvement, and, rarely, lung or heart problems.
Prevention Strategies of Cryoglobulinemia
There is no guaranteed way to prevent cryoglobulinemia, but strategies focus on managing underlying causes and avoiding triggers:
- Prevent Underlying Infections: Get vaccinated for Hepatitis B. Practice safe sex and avoid sharing needles to reduce the risk of Hepatitis C and HIV.
- Manage Associated Conditions: Effectively treating autoimmune diseases or blood cancers can prevent the development of cryoglobulinemia.
- Avoid Cold Exposure: This is the most direct way to prevent symptoms.
- Dress warmly in cold weather, wearing layers, gloves, thick socks, and hats.
- Avoid handling cold objects.
- In some cases, moving to a warmer climate may be considered.
Myths and Facts About Cryoglobulinemia
| Myth | Fact |
|---|---|
| Cryoglobulinemia is just a bad allergy to the cold. | It is not an allergy but an immune system disorder where proteins physically clump in the blood, blocking vessels and causing inflammation. |
| Only people with Hepatitis C get it. | While Hepatitis C is the most common cause, it can also be caused by other infections, autoimmune diseases, and cancers. |
| If you stay warm, the disease is cured. | Staying warm manages symptoms but does not address the underlying production of abnormal proteins or the associated disease. |
| It is a contagious disease. | Cryoglobulinemia itself is not contagious. However, the underlying cause (like Hepatitis C) can be. |
| There is no treatment available. | While there is no universal cure, many effective treatments exist to control the underlying condition, suppress the immune system, and remove the harmful proteins from the blood. |
Treatments and Therapy
Treatment is tailored to the severity of symptoms, the organs involved, and the underlying cause.
Medication-Based Treatments
- Antiviral Drugs: For Hepatitis C-related cryoglobulinemia, drugs like direct-acting antivirals (DAAs) are the first-line treatment to eradicate the virus.
- Corticosteroids: (e.g., Prednisone) to reduce rapid inflammation.
- Immunosuppressants: (e.g., Rituximab, Cyclophosphamide, Azathioprine) to control the overactive immune system and stop the production of cryoglobulins.
- Plasma Exchange (Plasmapheresis): A procedure to filter the cryoglobulins directly out of the blood, used in severe, life-threatening cases.
Surgical Treatments
Surgery is not a standard treatment for the condition itself but may be necessary for complications, such as debridement of severe skin ulcers or amputation for gangrenous limbs.
Lifestyle and Behavioral Interventions
As mentioned, strict cold avoidance is critical. Managing fatigue and joint pain through pacing and rest is also important.
Alternative and Complementary Medicine
No alternative therapies can treat cryoglobulinemia, but some patients find practices like acupuncture or mindfulness meditation helpful for managing pain and stress. These should always be used in addition to, not instead of, conventional medical care.
Immunizations and Vaccines
Staying up-to-date on vaccines is important, but live vaccines should be avoided if a patient is on strong immunosuppressants. Vaccination against Hepatitis B is a key preventive measure.
Stem Cell Therapy
This is an experimental and high-risk treatment reserved for the most severe, refractory cases where other treatments have failed, often in the context of an associated blood cancer.
Gene Therapy
Gene therapy is not currently a treatment option for cryoglobulinemia and remains in the realm of research.
Top 20 FAQ with Answers on Cryoglobulinemia
1. What is cryoglobulinemia in simple terms?
It’s a condition where abnormal proteins in your blood thicken and clump together when you’re cold, blocking small blood vessels and causing damage.
2. What is the main cause of cryoglobulinemia?
The most common cause is a chronic infection with the Hepatitis C virus.
3. Is cryoglobulinemia a form of cancer?
No, but one type (Type I) is often associated with blood cancers like multiple myeloma.
4. Is cryoglobulinemia an autoimmune disease?
It is considered an “immune-complex” mediated disease and is frequently linked to autoimmune disorders like Sjögren’s syndrome and lupus.
5. How is cryoglobulinemia diagnosed?
Through a blood test where the sample must be kept at body temperature until processed to detect the cryoglobulins. Other tests look for underlying causes and organ damage.
6. What does the cryoglobulinemia rash look like?
It typically appears as raised, purple-red spots called palpable purpura, most often on the lower legs.
7. Is there a cure for cryoglobulinemia?
There is no direct cure, but treating the underlying cause (like curing Hepatitis C) can often lead to remission of symptoms.
8. What is the life expectancy for someone with cryoglobulinemia?
It varies greatly. With mild disease, life expectancy can be normal. Severe disease with kidney or heart involvement can be serious, but modern treatments have significantly improved outcomes.
9. What should I avoid if I have cryoglobulinemia?
The most important thing to avoid is cold temperatures. You should also avoid smoking, as it worsens blood vessel constriction.
10. Can cryoglobulinemia affect the brain?
Direct central nervous system involvement is rare, but it can cause severe headaches, strokes, or bleeding in the brain in some cases.
11. Does cryoglobulinemia cause fatigue?
Yes, severe fatigue is one of the most common and debilitating symptoms.
12. What is the best treatment for cryoglobulinemia?
The “best” treatment depends on the cause. For Hepatitis C, it’s antiviral therapy. For severe immune-driven disease, it’s often Rituximab.
13. Can cryoglobulinemia go away on its own?
It is unlikely to resolve without treating the underlying condition.
14. What kind of doctor treats cryoglobulinemia?
Typically a rheumatologist or an immunologist, often in coordination with a hepatologist (for liver issues), nephrologist (for kidneys), or neurologist (for nerves).
15. Can you live a normal life with cryoglobulinemia?
Many people can manage their symptoms and live full lives by avoiding cold triggers and adhering to their treatment plan.
16. Does cryoglobulinemia run in families?
No, it is not considered a hereditary or genetic disorder.
17. Can it affect the heart?
Yes, though less common, it can cause inflammation of the heart arteries (coronary vasculitis) or heart muscle (myocarditis).
18. What is the difference between Type I, II, and III?
- Type I: Linked to cancer; single antibody; can cause severe blood vessel blockage.
- Type II & III: “Mixed” types; linked to Hepatitis C/autoimmune diseases; multiple antibodies; cause inflammation via immune complexes.
19. Why is it so important to keep the blood warm before testing?
If the blood sample cools, the cryoglobulins will clump and precipitate out, potentially being lost during processing and leading to a false-negative test result.
20. Is plasmapheresis a cure?
No, it is a temporary “clean-up” procedure to remove proteins during a crisis. It does not stop the body from producing new cryoglobulins.
Conclusion
Cryoglobulinemia is a complex and serious condition whose essence is the pathological cold-induced clumping of proteins in the blood. While its symptoms can be debilitating and range from a troublesome rash to life-threatening organ failure, significant progress has been made in understanding and treating it. The cornerstone of management involves a precise diagnosis, vigilant protection from cold, and most importantly, aggressive treatment of any underlying cause, such as the now-curable Hepatitis C. With a multidisciplinary medical approach, most patients can achieve good control of their disease and maintain a good quality of life.
Find Trusted Cardiac Hospitals
Compare heart hospitals by city and services — all in one place.
Explore Hospitals
This article does a great job explaining cryoglobulinemia in a way that’s both clear and practical, making it easier for readers to understand how cold‑sensitive proteins in the blood can lead to symptoms like joint pain, skin changes, and nerve issues. I appreciate the breakdown of different types and how they’re linked with underlying conditions, which helps put this complex blood disorder into perspective. The sections on diagnosis and management strategies are especially useful, as they offer realistic guidance on what to expect and how doctors approach treatment. Overall, it’s an informative and patient‑focused resource that raises awareness about a rare but important condition.