Introduction & Background of Maple Syrup Urine Disease (MSUD)
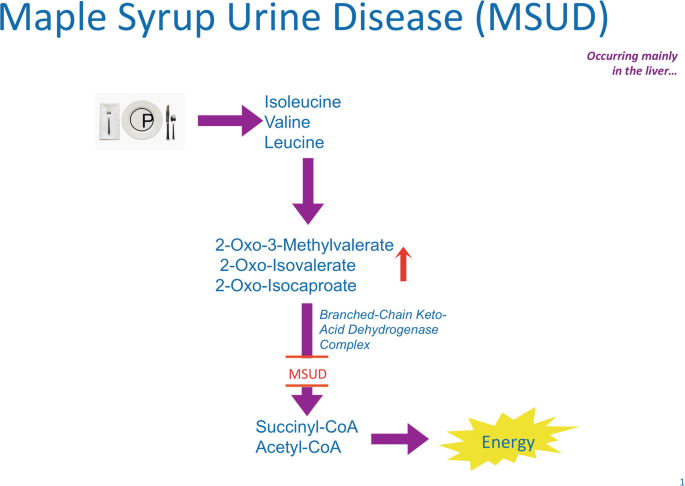
Maple Syrup Urine Disease (MSUD) is a rare, inherited metabolic disorder characterized by the body’s inability to properly break down certain amino acids, the building blocks of protein. Specifically, it affects the metabolism of the three branched-chain amino acids (BCAAs): leucine, isoleucine, and valine.
The name of the disorder comes from the distinctive sweet, maple syrup-like odor of the urine in affected infants. This odor is caused by the buildup of toxic byproducts from the incomplete breakdown of the BCAAs.
In a healthy individual, a complex of enzymes (the branched-chain alpha-keto acid dehydrogenase complex) processes these amino acids. In MSUD, this enzyme complex is either defective or missing entirely, leading to a dangerous accumulation of BCAAs and their toxic keto-acids in the blood and urine. This buildup is neurotoxic and can cause severe health complications, including brain damage, if not managed from birth.
Causes of Maple Syrup Urine Disease (MSUD)
MSUD is a genetic disorder, meaning it is caused by mutations in specific genes. It is inherited in an autosomal recessive pattern.
- Genetic Cause: Mutations in one of four genes: BCKDHA, BCKDHB, DBT, or DLD. These genes provide instructions for making the proteins that form the enzyme complex.
- Inheritance Pattern (Autosomal Recessive):
- A child must inherit two faulty copies of the gene (one from each parent) to have the disease.
- Parents of a child with MSUD are typically carriers. They have one working copy and one faulty copy of the gene, which allows them to produce enough of the enzyme to be healthy and asymptomatic.
- With each pregnancy, two carrier parents have a:
- 25% chance of having a child with MSUD.
- 50% chance of having a child who is a carrier like themselves.
- 25% chance of having a child with two working genes.
Indications and Symptoms of Maple Syrup Urine Disease (MSUD)
Symptoms of classic MSUD, the most common and severe form, typically appear within the first few days to weeks of life.
Early Signs in a Newborn (within 4-7 days):
- Poor feeding, fussiness, and lethargy.
- Vomiting and loss of appetite.
- The characteristic sweet, maple syrup odor in the earwax, sweat, and urine.
- Progressive neurological decline, including alternating periods of hypertonia (muscle stiffness) and hypotonia (floppy muscles).
- Abnormal, high-pitched cry.
Symptoms of a Metabolic Crisis (a medical emergency):
If undiagnosed and untreated, the condition rapidly progresses to a metabolic crisis, indicated by:
- Seizures
- Lethargy progressing to coma
- Respiratory distress
- Brain swelling (cerebral edema), which can be fatal.
Later-Onset Forms:
In milder, intermittent, or intermediate forms of MSUD, symptoms may not appear until later in infancy or childhood and are often triggered by illness, infection, surgery, or a high-protein meal.
Prevention Strategies of Maple Syrup Urine Disease (MSUD)
Because MSUD is a genetic condition, it cannot be “prevented” in the traditional sense. However, the severe consequences can be prevented through early detection and management.
- Newborn Screening (NBS): This is the primary prevention strategy for disability and death. In most developed countries, a heel-prick blood test is performed on newborns 24-48 hours after birth. This test measures the levels of leucine and other markers, allowing for diagnosis before symptoms appear.
- Genetic Counseling and Carrier Testing: For families with a known history of MSUD, genetic counseling is crucial. Carrier testing for at-risk relatives and prenatal diagnosis (via amniocentesis or chorionic villus sampling) are available options.
Myths and Facts About Maple Syrup Urine Disease (MSUD)
| Myth | Fact |
|---|---|
| Myth: Children with MSUD can never eat any protein. | Fact: They require a lifelong, carefully calculated diet that includes a small amount of natural protein to meet nutritional needs, supplemented by a special medical formula that provides all other amino acids and nutrients. |
| Myth: The “maple syrup” smell is harmless. | Fact: The smell is a direct indicator of a toxic buildup of BCAAs in the body and signifies that the person is at risk for a metabolic crisis. |
| Myth: MSUD only affects the diet. | Fact: It is a whole-body disorder. Metabolic stress from illness or injury can quickly become life-threatening, requiring an emergency protocol. It can also cause long-term neurological and developmental challenges if not perfectly managed. |
| Myth: It’s so rare I don’t need to worry about it. | Fact: While rare (affecting about 1 in 185,000 newborns globally), it is a core condition on newborn screening panels because early intervention is so effective. For families with a history, the risk is significantly higher. |
Treatments and Therapy
There is no cure for MSUD, but it is a manageable condition with lifelong, strict adherence to treatment. The goal is to maintain the levels of branched-chain amino acids (especially leucine) within a safe range.
Lifestyle and Behavioral Interventions (Primary Treatment)
- Dietary Management: This is the cornerstone of treatment.
- Medical Formula: A special formula free of leucine, isoleucine, and valine, but containing all other essential amino acids, vitamins, and minerals. This is the person’s primary source of nutrition.
- Limited Natural Protein: Intake of natural protein (from milk, meat, eggs, beans, nuts, and even regular flour) is strictly limited and calculated by a metabolic dietitian based on age, weight, and blood levels.
- Illness Management (Sick-Day Protocol): Even a minor cold can trigger a metabolic crisis. The protocol involves:
- Switching to an emergency diet of high-carbohydrate fluids and the special formula.
- Frequent monitoring of blood leucine levels.
- Seeking immediate medical attention for intravenous fluids if unable to eat or if levels rise dangerously.
Medication-Based Treatments
- Thiamine (Vitamin B1) Supplementation: In some rare, thiamine-responsive variants of MSUD, high doses of thiamine can help increase the activity of the defective enzyme complex.
Surgical Treatments
- Liver Transplantation: This is currently the closest thing to a cure. A transplanted liver produces a fully functional enzyme complex, allowing a person to tolerate a normal or near-normal diet. However, it carries the significant risks of lifelong immunosuppression to prevent organ rejection and the risks of the major surgery itself. It is considered for individuals with frequent metabolic crises despite strict dietary management.
Stem Cell Therapy & Gene Therapy
- Stem Cell Therapy: Liver transplantation is essentially a form of stem cell therapy (hepatocyte transplantation) has been explored but is not yet a standard treatment.
- Gene Therapy: This is an active area of research. The goal is to introduce a functional copy of the defective gene into the patient’s cells, potentially providing a permanent cure. While promising, it is not yet available as a clinical treatment.
(Note: Physical Therapy, Alternative Medicine, Psychotherapy, and Immunizations are not primary treatments for the core metabolic defect of MSUD, though supportive care like physical therapy may be used if developmental delays have occurred, and psychotherapy/counseling can support the mental health challenges of managing a chronic illness.)
Top 20 FAQ with Answers on Maple Syrup Urine Disease (MSUD)
1. What causes the maple syrup smell?
The smell comes from a compound called sotolone, which is a byproduct of the buildup of the branched-chain amino acid isoleucine.
2. Is MSUD curable?
There is no pharmaceutical cure yet. However, a liver transplant effectively “cures” the metabolic defect, allowing a normal diet, but requires lifelong immunosuppressant drugs.
3. Can a person with MSUD live a normal life?
Yes, with early diagnosis, strict lifelong dietary management, and careful monitoring during illness, individuals with MSUD can live long, relatively normal lives.
4. How is MSUD diagnosed?
It is primarily diagnosed through newborn blood spot screening. Confirmation is done through quantitative plasma amino acid analysis, which shows elevated levels of leucine, isoleucine, and valine.
5. What happens if someone with MSUD eats a high-protein meal?
It can cause a rapid rise in blood leucine levels, leading to toxicity, a metabolic crisis, and potential brain damage or death if not treated promptly.
6. Is MSUD contagious?
No, it is an inherited genetic disorder and cannot be caught from another person.
7. Can women with MSUD have children?
Yes, but it requires extremely careful management before and during pregnancy, under the guidance of a metabolic team. This is known as a “maternal MSUD” pregnancy.
8. What is a metabolic crisis?
A life-threatening medical emergency where toxic substances build up rapidly, causing vomiting, lethargy, seizures, coma, and brain swelling. It is often triggered by illness, infection, or skipping meals.
9. How often do blood levels need to be checked?
Frequency varies. In infancy, it may be several times a week. In a stable adult, it might be once a week or every two weeks. It is checked more frequently during illness or growth spurts.
10. Is the special formula enough to live on?
The special formula provides all necessary nutrients except for the three BCAAs. A small, calculated amount of natural food is added to the diet to provide just enough BCAAs for growth and repair without causing toxicity.
11. Are there different types of MSUD?
Yes. The main types are: Classic (most severe), Intermediate, Intermittent, Thiamine-responsive, and E3-Deficient (very rare).
12. What is the life expectancy for someone with MSUD?
With excellent metabolic control and access to modern medical care, life expectancy can be near normal.
13. Can you develop MSUD later in life?
No, it is a condition you are born with. However, milder forms may not be diagnosed until later infancy or childhood when a stressor (like an infection) triggers symptoms.
14. What should I do in an emergency?
Follow your emergency protocol: call your metabolic team and go to the hospital. Have a written letter from your doctor explaining MSUD and the need for IV fluids with high dextrose (sugar) and no electrolytes.
15. Does MSUD cause learning disabilities?
If not well-controlled, especially in early childhood, it can lead to intellectual and developmental disabilities. Good metabolic control minimizes this risk.
16. Is exercise safe for someone with MSUD?
Yes, but intense exercise can use protein for energy, potentially raising BCAA levels. It’s important to maintain good hydration and may require extra calories before exercise.
17. Can they ever eat sweets or treats?
Yes, many low-protein or protein-free specially manufactured foods, candies, and flours are available, allowing for a more varied diet.
18. Who is on the treatment team?
A metabolic specialist, metabolic dietitian, neurologist, genetic counselor, and often a psychologist or social worker.
19. Is there a support group?
Yes, organizations like the Maple Syrup Urine Disease Family Support Group and the National Urea Cycle Disorders Foundation provide vital resources, community, and support for families.
20. What is the most important thing to remember about managing MSUD?
Consistency is key. Strict, daily adherence to the diet and having a clear, proactive plan for managing illness are the pillars of staying healthy and preventing crises.
Conclusion
Maple Syrup Urine Disease is a profound and challenging metabolic disorder that demands constant vigilance. However, the advent of universal newborn screening has transformed the outlook for children born with MSUD. What was once a universally fatal condition is now a manageable chronic illness. Through a lifelong, protein-restricted diet, careful monitoring, and a robust partnership with a specialized metabolic team, individuals with MSUD can survive and thrive. Ongoing research into advanced therapies like gene therapy continues to offer hope for even better treatments and an improved quality of life in the future.
Find Trusted Cardiac Hospitals
Compare heart hospitals by city and services — all in one place.
Explore Hospitals
This guide on Maple Syrup Urine Disease makes a complex metabolic condition much easier to understand by clearly explaining how the body’s inability to break down certain amino acids leads to serious health issues. I appreciate the focus on early detection through newborn screening and the practical management strategies, especially the dietary approaches that are critical for preventing neurological damage. The article does a great job balancing medical accuracy with reader-friendly language, making it useful for families, caregivers, and anyone wanting to learn more about MSUD.