Introduction & Background of Stiff Person Syndrome – Muscle rigidity and spasms
Stiff Person Syndrome (SPS) is an exceptionally rare and progressive neurological disorder characterized by profound muscle stiffness and recurrent, painful spasms. It is often described as one of the most chronic and disabling human diseases. The hallmark of SPS is its impact on the central nervous system, specifically the brain and spinal cord, leading to a failure of normal inhibitory signals that control muscle movement.
The core problem in SPS is an autoimmune attack, where the body’s own immune system mistakenly targets a key enzyme called glutamic acid decarboxylase (GAD). GAD is essential for producing gamma-aminobutyric acid (GABA), the primary neurotransmitter responsible for putting the “brakes” on muscle activity. With reduced GABA, the muscles receive excessive excitatory signals, resulting in continuous contraction and stiffness.
SPS can affect anyone but is more common in women and often associated with other autoimmune conditions like type 1 diabetes, thyroiditis, and vitiligo. The severity can range from a relatively mild, localized form to a severe, widespread condition that significantly impairs mobility and quality of life.
Causes of Stiff Person Syndrome – Muscle rigidity and spasms
The exact cause of SPS is not fully understood, but it is predominantly considered an autoimmune disorder.
- Autoimmune Response: In approximately 60-80% of patients, the immune system produces antibodies that attack Glutamic Acid Decarboxylase (GAD antibodies). This disrupts the production of GABA, leading to uncontrolled muscle firing.
- Other Antibodies: Some patients may have antibodies against other proteins, such as amphiphysin or glycine receptors, which are also involved in inhibitory signaling.
- Paraneoplastic Syndrome: In rare cases, SPS can be a paraneoplastic syndrome, meaning it is triggered by an underlying cancer (e.g., breast cancer, lung cancer, Hodgkin’s lymphoma). The immune system’s reaction to the cancer mistakenly attacks nerve cells.
- Idiopathic: For a small subset of patients, no specific antibody or underlying cause can be identified.
Indications of Stiff Person Syndrome – Muscle rigidity and spasms
“Indications” often refer to signs that lead to a diagnosis. Key indicators of SPS include:
- Progressive Stiffness: A gradual onset of stiffness, typically beginning in the trunk and abdominal muscles.
- Painful Spasms: Episodes of severe muscle spasms that are often triggered by unexpected noises, light touch, emotional distress, or sudden movement.
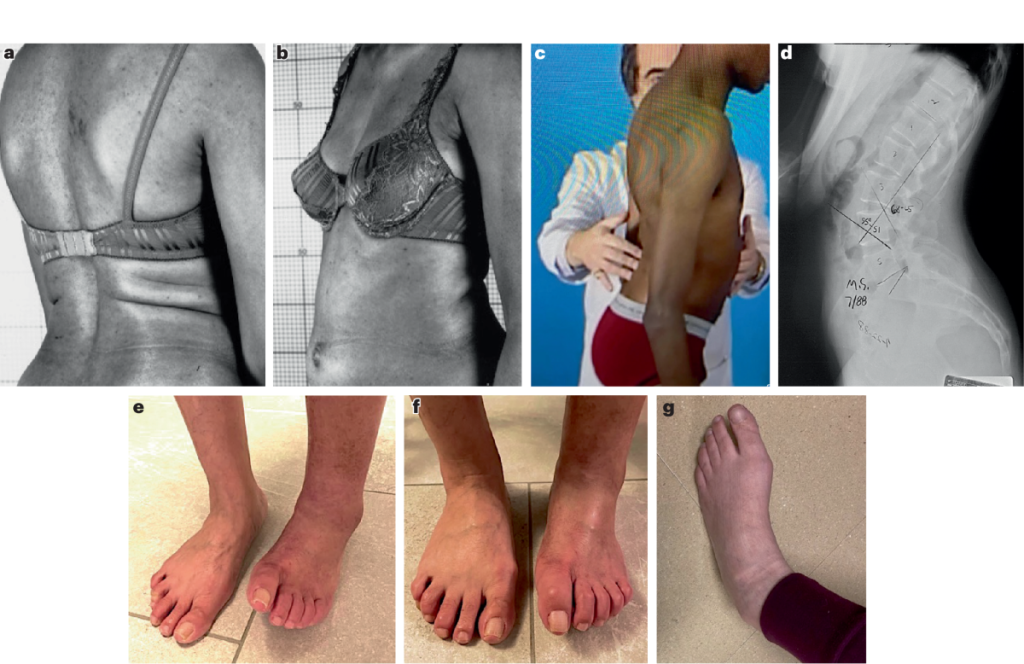
- Abnormal Posture: A rigid, board-like abdomen and a hunched-over or hyper-extended posture due to continuous muscle contraction.
- Gait Difficulties: A stiff, slow, and wide-based gait, often described as “walking like a tin soldier.”
- Co-existing Autoimmune Conditions: The presence of other autoimmune diseases, such as type 1 diabetes or thyroiditis, can be a strong indicator.
Symptoms of Stiff Person Syndrome – Muscle rigidity and spasms
Symptoms vary but typically include:
- Muscle Rigidity: Constant, painful stiffness in the trunk, legs, and sometimes shoulders and neck.
- Muscle Spasms: Violent, painful spasms that can last for minutes or hours. These can be strong enough to fracture bones or dislocate joints.
- Exaggerated Startle Response: An extreme reaction to sudden stimuli.
- Postural Deformities: Severe lumbar lordosis (swayback) or a fixed, hunched posture.
- Heightened Anxiety: Many patients develop a fear of falling or leaving the house (agoraphobia) because they know environmental triggers can cause debilitating spasms. This anxiety is a direct consequence of the physical condition.
- Functional Impairment: Difficulty walking, bending, or performing daily tasks. In advanced stages, patients may become bedridden.
Prevention Strategies of Stiff Person Syndrome – Muscle rigidity and spasms
As an autoimmune disorder with no known cause, SPS cannot be prevented. However, the focus is on preventing complications and worsening of symptoms:
- Trigger Management: Identifying and avoiding personal triggers (e.g., loud noises, cold environments, stress) can help prevent spasms.
- Fall Prevention: Using assistive devices (canes, walkers) and making home modifications (handrails, non-slip mats) to prevent falls and injuries.
- Stress Management: Engaging in relaxation techniques like meditation, deep breathing, or gentle yoga to minimize stress-induced symptoms.
- Prompt Medical Care: Seeking early diagnosis and treatment to manage the autoimmune process and slow disease progression.
Myths and Facts About Stiff Person Syndrome – Muscle rigidity and spasms
| Myth | Fact |
|---|---|
| SPS is a muscle disease. | SPS is a neurological disorder originating in the central nervous system. |
| It’s a form of Parkinson’s. | While both affect movement, they are distinct diseases with different causes and pathologies. |
| SPS is psychosomatic or “all in your head.” | SPS is a very real, physical disease with identifiable biological markers (e.g., GAD antibodies). The anxiety is a common symptom, not the cause. |
| It’s contagious. | SPS is an autoimmune disorder and is not infectious or contagious in any way. |
| Everyone with SPS has the same symptoms. | Symptoms and severity vary widely. Some have a localized form (e.g., stiff leg syndrome), while others have widespread involvement. |
Treatments and Therapy
There is no cure for SPS, so treatment focuses on managing symptoms, reducing spasms, and improving mobility and quality of life.
Medication-Based Treatments
- Benzodiazepines: (e.g., Diazepam/Valium, Clonazepam) are first-line treatments. They enhance GABA’s effect, directly countering the core problem.
- Muscle Relaxants: (e.g., Baclofen) help reduce muscle stiffness and spasms.
- Immunotherapies: Intravenous Immunoglobulin (IVIG) is a primary immunotherapy that modulates the immune system. Rituximab and other immunosuppressants (e.g., Mycophenolate) may also be used.
- Corticosteroids: (e.g., Prednisone) can be used to quickly suppress immune activity.
Surgical Treatments
Surgery is not a standard treatment for SPS itself. However, Intrathecal Baclofen (ITB) Therapy, which involves surgically implanting a pump to deliver baclofen directly into the spinal fluid, can be highly effective for severe, treatment-resistant cases.
Physical Therapy and Rehabilitation
Crucial for maintaining function. Focuses on gentle stretching, range-of-motion exercises, hydrotherapy, and gait training to prevent contractures and improve mobility.
Lifestyle and Behavioral Interventions
- Heat Therapy: Warm baths or heating pads can temporarily relax stiff muscles.
- Stress Reduction: Mindfulness, meditation, and avoiding stressful situations.
- Pacing Activities: Learning to balance activity with rest to avoid fatigue-triggered spasms.
Alternative and Complementary Medicine
- Acupuncture: May help some patients manage pain and muscle tension.
- Massage Therapy: Gentle massage can provide temporary relief from stiffness.
- Note: These should be used as complements to, not replacements for, standard medical care.
Psychotherapy and Counseling
Essential for coping with the chronic, unpredictable nature of the disease. Therapy can help manage anxiety, depression, and the fear associated with spasms and falls.
Immunizations and Vaccines
There is no vaccine to prevent SPS. The relationship between vaccines and autoimmune flares is complex and patient-specific; decisions should be made in consultation with a neurologist.
Stem Cell Therapy
An experimental treatment where the patient’s immune system is “rebooted” using hematopoietic stem cells. It is being studied in clinical trials for severe, refractory SPS but is not yet a standard treatment.
Gene Therapy
Currently, gene therapy is not a treatment option for SPS and remains in the realm of theoretical research.
Top 20 FAQ with answer on Stiff Person Syndrome – Muscle rigidity and spasms
1. What is Stiff Person Syndrome (SPS)?
A rare neurological disorder causing severe muscle stiffness and spasms due to an autoimmune attack on the nervous system.
2. Is SPS fatal?
While SPS itself is not typically fatal, serious complications like uncontrolled spasms, falls, or autonomic dysfunction can be life-threatening if not properly managed.
3. How is SPS diagnosed?
Through a combination of clinical examination, blood tests for GAD antibodies (and others), and electromyography (EMG) which shows continuous motor unit activity.
4. What is the life expectancy for someone with SPS?
With modern treatments, many patients can have a near-normal life expectancy, though quality of life is significantly impacted.
5. Is there a cure for SPS?
No, there is no cure, but symptoms can be effectively managed with a combination of medications and therapies.
6. What triggers SPS spasms?
Common triggers include sudden noise, light touch, emotional stress, cold temperatures, and unexpected movement.
7. Is SPS a form of Multiple Sclerosis (MS)?
No, they are distinct autoimmune disorders, though they can share some similar neurological symptoms.
8. Can children get SPS?
Yes, though it is extremely rare, a pediatric form of SPS exists.
9. Does SPS affect cognitive function?
SPS does not typically cause dementia or major cognitive decline. However, chronic pain, anxiety, and sleep deprivation can affect concentration and memory.
10. Can you work with SPS?
It depends on the severity. Many patients can work, often with accommodations, while those with severe symptoms may be unable to.
11. Is SPS considered a disability?
Yes, due to its profound impact on mobility and daily function, SPS is recognized as a disability.
12. What is the difference between SPS and Fibromyalgia?
Fibromyalgia causes widespread pain and tenderness but not the same degree of measurable, continuous muscle rigidity and spasms seen in SPS.
13. Can physical therapy make SPS worse?
If done aggressively, yes. It must be performed by a therapist familiar with SPS, using gentle, pain-free techniques.
14. What is the first-line treatment for SPS?
Benzodiazepines like diazepam are often the first medication used to increase GABA activity and reduce symptoms.
15. How common is SPS?
It is extremely rare, affecting approximately 1 or 2 people per million.
16. Can SPS go into remission?
Spontaneous remission is very rare. However, with effective immunotherapy, symptoms can be significantly suppressed for long periods.
17. Does diet affect SPS?
There is no specific “SPS diet,” but a healthy, anti-inflammatory diet may support overall well-being. Some patients find that caffeine or sugar can exacerbate symptoms.
18. Can stress cause SPS?
Stress does not cause SPS, but it is a major trigger for worsening symptoms and spasms.
19. What specialist treats SPS?
A neurologist, ideally one with expertise in autoimmune or movement disorders.
20. What is the latest research on SPS?
Research is focused on understanding the autoimmune mechanisms, developing more targeted immunotherapies, and exploring the potential of treatments like stem cell therapy.
Conclusion
Stiff Person Syndrome is a complex, challenging, and often misunderstood neurological disorder. Its hallmark—severe rigidity and spasms—stems from an autoimmune disruption of the brain’s fundamental inhibitory systems. While there is no cure, a multifaceted approach combining immunotherapies, symptom-relieving medications, physical rehabilitation, and psychological support can provide significant relief and help patients regain a degree of control over their lives. Increased awareness and ongoing research are crucial to improving diagnostics, developing more effective treatments, and ultimately finding a cure for this debilitating condition.
Find Trusted Cardiac Hospitals
Compare heart hospitals by city and services — all in one place.
Explore Hospitals