Introduction & Background of Alpha-1 Antitrypsin Deficiency – Affects Lungs and Liver
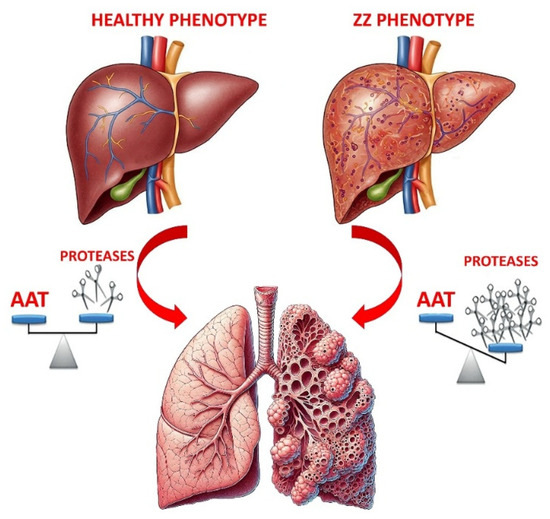
Alpha-1 Antitrypsin Deficiency (Alpha-1) is a genetic, inherited disorder that significantly increases the risk of developing lung and liver disease. It is caused by a mutation in the SERPINA1 gene, which provides instructions for making the Alpha-1 antitrypsin (AAT) protein. This protein is produced in the liver and its primary role is to protect the body’s tissues, especially the lungs, from being damaged by neutrophil elastase—a powerful enzyme released by white blood cells to fight infection.
In Alpha-1, the AAT protein is misfolded and becomes trapped in the liver cells. This leads to a double-hit effect:
- Low AAT levels in the blood: The lungs are left vulnerable to attack by neutrophil elastase, which slowly destroys the alveoli (air sacs), leading to emphysema and COPD.
- AAT accumulation in the liver: The buildup of the abnormal protein causes liver cell damage, inflammation, and scarring (fibrosis), which can progress to cirrhosis and liver failure.
Causes of Alpha-1 Antitrypsin Deficiency – Affects Lungs and Liver
Alpha-1 is an autosomal co-dominant genetic condition. This means:
- You must inherit a defective gene from both parents to have the severe form of the deficiency.
- If you inherit one defective gene, you are a “carrier.” Carriers may have slightly lower AAT levels but are generally not at high risk for severe disease, though some studies suggest a possible increased risk, especially if they smoke.
The most common abnormal variants are labeled S and Z. The PiMM genotype is normal. The most severe deficiency is seen in the PiZZ genotype. The PiMZ genotype indicates a carrier state.
Indications of Alpha-1 Antitrypsin Deficiency – Affects Lungs and Liver
When to suspect and test for Alpha-1:
- Lung Indications:
- Emphysema or COPD in a person before the age of 45.
- COPD in an individual who has never smoked or had minimal smoke exposure.
- A family history of COPD, emphysema, or liver disease.
- Asthma that is not fully reversible with aggressive treatment.
- Unexplained liver disease in both children and adults.
- A specific pattern of emphysema on a CT scan that shows damage primarily in the lower lobes of the lungs.
- Liver Indications:
- Unexplained chronic hepatitis or cirrhosis.
- Liver cancer (hepatocellular carcinoma).
- A family history of liver disease.
- Jaundice (yellowing of the skin and eyes) in infancy.
Symptoms of Alpha-1 Antitrypsin Deficiency – Affects Lungs and Liver
Lung-Related Symptoms (often appear between ages 20-50):
- Shortness of breath, initially during activity and later at rest
- Chronic cough, often with phlegm (sputum) production
- Wheezing and a whistling sound when breathing
- Recurring respiratory infections
- Reduced ability to exercise
- Fatigue and general weakness
- Barrel-shaped chest (in advanced emphysema)
Liver-Related Symptoms:
- In Infants: Jaundice, swollen abdomen, poor feeding, failure to thrive.
- In Adults: Fatigue, loss of appetite, weight loss, swelling in the legs (edema) or abdomen (ascites), jaundice, easy bruising or bleeding.
Prevention Strategies of Alpha-1 Antitrypsin Deficiency – Affects Lungs and Liver
Since Alpha-1 is genetic, the condition itself cannot be prevented. However, the onset and progression of associated diseases can be dramatically slowed.
- Do Not Smoke: This is the single most important action. Smoking massively accelerates lung damage.
- Avoid Lung Irritants: Stay away from secondhand smoke, dust, fumes, and air pollution. Wear a mask if necessary.
- Limit or Avoid Alcohol: Alcohol can stress the liver, which is already compromised by the accumulation of abnormal AAT protein.
- Get Vaccinated: Protect against respiratory infections (influenza, pneumococcal pneumonia) and liver infections (Hepatitis A and B).
- Genetic Counseling: For individuals with a family history, genetic counseling can help understand the risks of passing the gene to children.
Myths and Facts About Alpha-1 Antitrypsin Deficiency – Affects Lungs and Liver
| Myth | Fact |
|---|---|
| Alpha-1 is a rare disease. | It is one of the most common genetic disorders, but it is widely underdiagnosed. Many people are misdiagnosed with asthma or “smoker’s COPD.” |
| Only people who smoke get lung disease from Alpha-1. | While smoking drastically worsens it, non-smokers with Alpha-1 can still develop significant lung disease. |
| If you’re just a carrier (PiMZ), there’s no risk. | Carriers may have a slightly increased risk of lung and liver disease, especially if they have other risk factors like smoking. |
| Alpha-1 only affects the lungs. | It is a multi-system disease primarily affecting the lungs and liver. It is also associated with a skin condition called panniculitis and certain types of vasculitis. |
| There is no treatment. | While there is no cure, there is a specific treatment called Augmentation Therapy to slow lung damage. Other treatments manage symptoms and complications. |
Treatments and Therapy
There is no cure for Alpha-1, but treatment focuses on slowing disease progression, managing symptoms, and preventing complications.
Medication-Based Treatments
- Augmentation Therapy: The primary specific treatment. It involves weekly IV infusions of purified AAT protein from donor plasma to raise the level in the blood and protect the lungs.
- Bronchodilators: Inhaled medications (like albuterol) that help open the airways.
- Inhaled Corticosteroids: Reduce inflammation in the airways.
- Antibiotics: To treat acute respiratory infections promptly.
Surgical Treatments
- Lung Volume Reduction Surgery: Removal of damaged portions of the lung to help the healthier parts work better.
- Lung Transplant: For patients with end-stage lung disease.
- Liver Transplant: The only cure for end-stage liver disease caused by Alpha-1. It also corrects the metabolic defect, as the new liver produces normal AAT protein.
Physical Therapy and Rehabilitation
- Pulmonary Rehabilitation: A cornerstone of management. Includes exercise training, breathing techniques, and education to improve daily function and quality of life.
Lifestyle and Behavioral Interventions
- Smoking cessation, alcohol avoidance, a balanced diet, and regular, moderate exercise as tolerated.
Alternative and Complementary Medicine
- Some patients find techniques like yoga, tai chi, and acupuncture helpful for stress management and improving breath control. These should complement, not replace, standard medical care.
Psychotherapy and Counseling
- A chronic illness like Alpha-1 can lead to anxiety, depression, and social isolation. Counseling and support groups are vital for mental and emotional health.
Immunizations and Vaccines
- Crucial for preventing illnesses that can severely worsen lung and liver health. Key vaccines include Flu, Pneumococcal, COVID-19, and Hepatitis A & B.
Stem Cell Therapy
- Still experimental. The goal would be to use stem cells to generate healthy liver cells that can produce normal AAT.
Gene Therapy
- The ultimate goal for a cure. Research is ongoing to deliver a normal copy of the SERPINA1 gene into the patient’s cells, allowing the body to produce its own functional AAT protein. It is not yet a clinical reality.
Top 20 FAQ with Answer on Alpha-1 Antitrypsin Deficiency – Affects Lungs and Liver
1. What is Alpha-1 Antitrypsin Deficiency?
It is an inherited genetic disorder that causes low levels of a protein (AAT) that protects the lungs, leading to emphysema and COPD. The abnormal protein can also build up in the liver, causing liver disease.
2. How is Alpha-1 inherited?
It is passed down from parents to children. To have the severe form, you must inherit one defective gene from each parent.
3. If I am a carrier (have one gene), will I get sick?
Most carriers do not get severely sick, but they may have a slightly higher risk for lung and liver problems, especially if they smoke or have other risk factors.
4. What are the first signs of Alpha-1?
The earliest signs are often shortness of breath with mild activity, a chronic cough, or wheezing. In babies, the first sign can be jaundice.
5. Is there a cure for Alpha-1?
There is no cure, but specific treatments like augmentation therapy can slow lung damage. A liver transplant can cure the liver aspect of the disease.
6. What is augmentation therapy?
It is a weekly IV infusion of purified AAT protein to boost the level in your blood and help protect your lungs from further damage.
7. Who should be tested for Alpha-1?
Anyone with COPD, emphysema, asthma that doesn’t fully respond to treatment, unexplained liver disease, or a family history of these conditions.
8. How is Alpha-1 diagnosed?
A simple blood test that measures the level of AAT in your blood. If low, a follow-up “phenotype” or “genotype” test identifies the specific genetic variants.
9. Can children have Alpha-1?
Yes. They can present with liver disease in infancy. Lung disease typically develops in adulthood.
10. Why does Alpha-1 affect the liver?
The abnormal AAT protein is misfolded and gets stuck in the liver cells where it’s made. This accumulation is toxic and leads to scarring (cirrhosis) over time.
11. Can I drink alcohol if I have Alpha-1?
It is generally recommended to limit or avoid alcohol, as it places additional stress on the liver.
12. Is it safe to exercise?
Yes, exercise is encouraged as part of pulmonary rehabilitation. It improves cardiovascular fitness and muscle strength, making daily activities easier.
13. Will I need a lung or liver transplant?
Not everyone will. Transplants are reserved for end-stage disease when other treatments are no longer effective.
14. What is the life expectancy for someone with Alpha-1?
It varies greatly. With early diagnosis, avoidance of smoking, and appropriate treatment, many people have a normal or near-normal life expectancy.
15. If I have Alpha-1, what are the chances my children will have it?
If your partner is not a carrier, your children will all be carriers. If your partner is also a carrier, each child has a 25% chance of having Alpha-1, a 50% chance of being a carrier, and a 25% chance of being unaffected.
16. What is the difference between Alpha-1 and COPD?
COPD is a broad term for lung diseases like emphysema and chronic bronchitis. Alpha-1 is a specific genetic cause of COPD.
17. Does Alpha-1 cause asthma?
No, but it can cause asthma-like symptoms (wheezing, shortness of breath), and people with Alpha-1 can also have coincidental asthma.
18. Are there any dietary recommendations?
A well-balanced, nutritious diet is important. If you have liver disease, your doctor may recommend a low-sodium diet to manage fluid retention.
19. Can the lung damage be reversed?
No, the damage to the lung tissue (emphysema) is permanent. Treatment aims to stop further damage and manage symptoms.
20. Where can I find support?
Organizations like the Alpha-1 Foundation and the Alpha-1 Association provide excellent resources, support networks, and information for patients and families.
Conclusion
Alpha-1 Antitrypsin Deficiency is a significant but often overlooked genetic disorder with serious consequences for the lungs and liver. While the genetic defect cannot be reversed, the trajectory of the disease can be profoundly altered. Early diagnosis through increased awareness and testing is critical. A comprehensive management plan—including smoking cessation, avoidance of environmental triggers, augmentation therapy where indicated, vaccinations, pulmonary rehabilitation, and strong psychosocial support—can empower individuals with Alpha-1 to live longer, healthier, and more active lives. Ongoing research into gene and stem cell therapies continues to offer hope for more definitive treatments in the future.
Find Trusted Cardiac Hospitals
Compare heart hospitals by city and services — all in one place.
Explore Hospitals
Alpha-1 antitrypsin deficiency is one of those conditions where awareness can genuinely change outcomes, because early testing and lifestyle choices can slow lung damage and protect the liver before symptoms become severe. What makes this guide useful is the clear connection between genetics and real-life risk—why some people develop early COPD-like breathing problems or unexplained liver issues, and why smoking, secondhand smoke, and occupational dust can accelerate harm. It also reinforces a smart patient approach: confirm diagnosis with proper blood tests and genotyping, screen family members when appropriate, stay up to date on vaccines, and work with a specialist to decide whether treatments like augmentation therapy fit your situation. Most importantly, it helps readers understand that “rare” doesn’t mean “hopeless”—with the right follow-up plan, lung care, liver monitoring, and prevention, many people can maintain a good quality of life for years.