Introduction & Background of Behçet’s Disease – Blood vessel inflammation
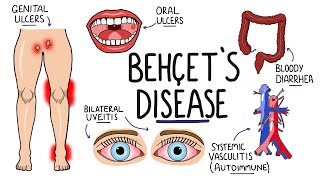
Behçet’s Disease, also known as Behçet’s Syndrome, is a rare, chronic, and complex autoimmune disorder characterized by widespread inflammation of the blood vessels (vasculitis). This inflammation can affect arteries and veins of all sizes, leading to a vast and unpredictable array of symptoms that can seem unrelated at first glance.
The disease is named after Dr. Hulusi Behçet, a Turkish dermatologist who first formally described it in 1937. At its core, Behçet’s is a multisystemic condition, meaning it can impact many organ systems, including the skin, mucous membranes, eyes, joints, digestive tract, and nervous system. The primary hallmark is the presence of recurrent oral and genital ulcers. The course of the disease is variable, often marked by periods of flare-ups and remission. Its exact cause remains unknown, but it is believed to involve a combination of genetic predisposition and environmental triggers.
Causes of Behçet’s Disease – Blood vessel inflammation
The precise cause of Behçet’s Disease is not fully understood. It is considered an autoinflammatory disorder, where the body’s immune system mistakenly attacks its own healthy cells and tissues, primarily targeting the blood vessels. The leading theory involves a two-hit process:
- Genetic Predisposition: The presence of a specific gene, HLA-B51, is strongly associated with an increased risk of developing Behçet’s, particularly in people from the Middle East and East Asia. However, having the gene does not guarantee one will get the disease, and many without the gene can still develop it.
- Environmental Trigger: In genetically susceptible individuals, an environmental trigger is thought to initiate the abnormal immune response. Potential triggers include:
- Infections: Certain bacteria (e.g., Streptococcus sanguinis) or viruses have been suspected.
- Autoimmune Reaction: The immune system may cross-react, attacking healthy tissues after an infection.
- Other Factors: Unknown environmental chemicals or other factors may also play a role.
The result is a dysregulated immune response with elevated levels of inflammatory cytokines like TNF-alpha, leading to neutrophil hyperreactivity and the characteristic blood vessel inflammation.
Indications of Behçet’s Disease – Blood vessel inflammation
“Indications” often refer to signs that point toward a diagnosis. Since there is no single definitive test for Behçet’s, diagnosis is based on a set of clinical criteria. The International Criteria for Behçet’s Disease (ICBD) requires a point score, with key indications including:
- Recurrent Oral Ulcers (2 points): Minor, major, or herpetiform ulcers that recur at least three times in a 12-month period.
- Recurrent Genital Ulcers (2 points): Typically painful and scarring.
- Eye Lesions (2 points): Anterior or posterior uveitis, or retinal vasculitis.
- Skin Lesions (1 point): Such as erythema nodosum, pseudofolliculitis, or acne-like nodules.
- Vascular Manifestations (1 point): Evidence of blood vessel involvement like thrombosis (blood clots), aneurysms, or superficial phlebitis.
- Positive Pathergy Test (1 point): An exaggerated skin reaction to a minor needle prick, though this is less common in patients from North America and Europe.
A score of 4 or more points is suggestive of Behçet’s Disease.
Symptoms of Behçet’s Disease – Blood vessel inflammation
Symptoms vary greatly from person to person and can come and go. They are a direct result of inflammation in various blood vessels.
- Mucocutaneous (Mouth and Skin):
- Mouth Sores: Painful canker sores on the tongue, gums, and inside of the cheeks.
- Genital Sores: On the scrotum or vulva; often painful and may scar.
- Skin Lesions: Red, tender nodules on legs (erythema nodosum), acne-like sores, or red bumps after minor trauma (pathergy).
- Ocular (Eyes):
- Redness, pain, blurred vision, floaters, and sensitivity to light.
- Can lead to serious complications like uveitis, retinal vasculitis, and potential blindness if untreated.
- Musculoskeletal (Joints):
- Arthritis, causing pain, swelling, and stiffness in the knees, ankles, wrists, and elbows.
- Vascular (Blood Vessels):
- Inflammation in veins can cause blood clots (thrombophlebitis), often in the legs.
- Inflammation in arteries can lead to aneurysms (weakening and bulging of the artery wall), which can be life-threatening.
- Neurological (Central Nervous System – “Neuro-Behçet’s”):
- Headaches, confusion, strokes, personality changes, and meningitis-like symptoms.
- Gastrointestinal (Digestive Tract – “Gut-Behçet’s”):
- Abdominal pain, diarrhea, bleeding, and ulcers that can mimic Crohn’s disease.
- Other: Fatigue, fever, and general malaise are common during flares.
Prevention Strategies of Behçet’s Disease – Blood vessel inflammation
There is no known way to prevent the onset of Behçet’s Disease itself, as the cause is not fully understood. However, the focus is on preventing flares and complications:
- Adherence to Medication: Consistently taking prescribed immunosuppressive or biologic drugs is the most effective way to prevent inflammation and flares.
- Lifestyle Management: Reducing stress, getting adequate rest, and maintaining a balanced diet can help manage the immune system.
- Oral Hygiene: Using soft toothbrushes and avoiding harsh mouthwashes may reduce trauma that triggers mouth ulcers.
- Regular Medical Monitoring: Frequent check-ups with a rheumatologist and other specialists (ophthalmologist, neurologist, etc.) are crucial for early detection and management of complications.
- Avoiding Known Triggers: For some, specific foods or stressors may provoke symptoms; identifying and avoiding these can help.
Myths and Facts About Behçet’s Disease – Blood vessel inflammation
| Myth | Fact |
|---|---|
| Behçet’s is contagious. | False. It is an autoimmune disorder, not an infection. You cannot catch it from another person. |
| It only affects people of Middle Eastern or Asian descent. | False. While it is more common along the ancient “Silk Road,” it can affect people of all ethnicities and nationalities. |
| Behçet’s is just a “sore disease.” | False. The sores are a visible symptom, but the underlying systemic vasculitis can damage vital organs like the eyes, brain, and blood vessels. |
| There is no treatment for Behçet’s. | False. While there is no cure, many effective treatments can control symptoms, reduce inflammation, and prevent serious complications. |
| People with Behçet’s cannot live a normal life. | False. With proper treatment and management, many people with Behçet’s lead full, active, and productive lives. |
| It’s a form of herpes. | False. The ulcers are not caused by the herpes virus. They are a result of autoinflammatory vasculitis. |
Treatments and Therapy
Treatment is tailored to the individual’s symptoms and organ involvement, with the goal of reducing inflammation, controlling pain, and preventing serious complications.
Medication-Based Treatments
- Corticosteroids: (e.g., Prednisone) Used to rapidly control severe inflammation during acute flares.
- Immunosuppressants: (e.g., Azathioprine, Cyclosporine, Cyclophosphamide) Used to control the disease long-term and reduce steroid dependence.
- Biologics: (e.g., TNF-alpha inhibitors like Infliximab, Adalimumab, Etanercept; Interleukin inhibitors) Target specific parts of the immune system and are highly effective for severe, refractory cases, especially for eye and central nervous system involvement.
- Colchicine: Often used for joint and skin symptoms, particularly erythema nodosum.
- Topical Therapies: Corticosteroid gels or rinses for mouth and genital ulcers to reduce pain and inflammation.
Surgical Treatments
Surgery is not a treatment for Behçet’s itself but may be necessary for complications.
- Vascular Surgery: To repair aneurysms or address major blood clots.
- Bowel Resection: To remove perforated or bleeding intestinal ulcers.
- Eye Surgery: For complications like cataracts or glaucoma caused by chronic inflammation.
Physical Therapy and Rehabilitation
Can help maintain joint mobility and muscle strength in patients with chronic arthritis.
Lifestyle and Behavioral Interventions
- Stress Management: Yoga, meditation, and counseling.
- Regular, Low-Impact Exercise: Such as swimming or walking.
- Balanced Diet: No specific diet for Behçet’s, but a healthy, anti-inflammatory diet can support overall well-being.
Alternative and Complementary Medicine
- Acupuncture: May help with pain management for some.
- Dietary Supplements: Like omega-3 fatty acids, which have anti-inflammatory properties. (Always consult a doctor before starting supplements).
Psychotherapy and Counseling
Essential for coping with the emotional and psychological challenges of a chronic, unpredictable illness, such as depression, anxiety, and social isolation.
Immunizations and Vaccines
Patients on immunosuppressants should generally avoid live vaccines. It is crucial to discuss vaccination schedules with a rheumatologist. Annual flu shots and pneumonia vaccines (inactivated) are typically recommended.
Stem Cell Therapy
An experimental and high-risk treatment reserved for the most severe, life-threatening cases that have not responded to any other therapy. It aims to “reboot” the immune system.
Gene Therapy
Currently in the realm of theoretical research for Behçet’s, exploring ways to correct the underlying genetic dysregulation that contributes to the disease.
Top 20 FAQ with answer on Behçet’s Disease – Blood vessel inflammation
- What is Behçet’s Disease?
It is a chronic autoimmune disorder causing inflammation of the blood vessels (vasculitis) throughout the body. - Is Behçet’s Disease contagious?
No, it is not contagious. You cannot catch it from someone else. - What causes Behçet’s Disease?
The cause is unknown, but it is believed to be a combination of genetic predisposition (like the HLA-B51 gene) and an environmental trigger. - Is Behçet’s Disease fatal?
While it is a serious disease, it is rarely fatal with proper treatment. Severe complications involving major blood vessels or the central nervous system can be life-threatening. - How is Behçet’s Disease diagnosed?
There is no single test. Diagnosis is based on a set of international clinical criteria, including recurrent oral/genital ulcers, eye inflammation, skin lesions, and a positive pathergy test. - What is a pathergy test?
A test where a small, sterile needle prick is made on the skin. A positive result is the formation of a red bump or pustule 24-48 hours later, indicating skin hypersensitivity. - Who gets Behçet’s Disease?
It can affect anyone, but it is most common in people from the Middle East, the Mediterranean, and East Asia (the “Silk Road”). Men and women are affected, but it is often more severe in men. - Is there a cure for Behçet’s Disease?
There is currently no cure, but treatments can effectively manage symptoms and control the disease. - What are the most common symptoms?
The most common are recurrent mouth sores, genital sores, skin rashes, and eye inflammation. - How does Behçet’s affect the eyes?
It can cause uveitis and retinal vasculitis, leading to pain, redness, blurred vision, and if untreated, permanent vision loss. - Can Behçet’s affect the brain?
Yes, this is called Neuro-Behçet’s. It can cause headaches, meningitis, strokes, and confusion. - What kind of doctor treats Behçet’s Disease?
A rheumatologist typically coordinates care, but a team of specialists (ophthalmologist, dermatologist, neurologist, etc.) is often involved. - What treatments are available?
Treatments range from corticosteroids and immunosuppressants (like azathioprine) to biologic drugs (like TNF-alpha inhibitors). - Can diet affect Behçet’s Disease?
There is no proven “Behçet’s diet,” but some patients find that certain foods trigger their mouth ulcers. A healthy, balanced diet is recommended for overall health. - Can I have children if I have Behçet’s?
Yes, but it requires careful planning. Pregnancy should be timed during a period of disease remission, and medications may need to be adjusted under a doctor’s supervision. - Does Behçet’s Disease affect life expectancy?
For most patients with well-controlled disease, life expectancy is normal. - Why do my symptoms come and go?
Behçet’s is characterized by unpredictable periods of flare-ups (when symptoms are active) and remission (when symptoms disappear or lessen). - Is fatigue a common symptom?
Yes, severe fatigue is extremely common, both from the disease itself and as a side effect of medications. - Are there support groups for Behçet’s patients?
Yes, organizations like the American Behçet’s Disease Association (ABDA) offer valuable resources, support, and community connections. - What is the long-term outlook for someone with Behçet’s?
The outlook is highly variable. Many patients can achieve good control with medication and live full lives. The course of the disease often becomes less severe over time.
Conclusion
Behçet’s Disease is a formidable and unpredictable challenge, defined by its systemic inflammation of blood vessels. While its origins remain partially elusive, significant strides have been made in understanding its genetic and immunological underpinnings. The absence of a cure is counterbalanced by a growing arsenal of effective treatments, from conventional immunosuppressants to advanced biologic therapies, which can dramatically improve quality of life and prevent devastating complications. A diagnosis of Behçet’s necessitates a proactive, lifelong partnership between the patient and a multidisciplinary medical team. Through continued research, increased awareness, and comprehensive care, the journey with Behçet’s can be successfully managed, empowering patients to lead fulfilling lives despite the disease.
Find Trusted Cardiac Hospitals
Compare heart hospitals by city and services — all in one place.
Explore Hospitals
This guide explains Behcet’s Disease in a very clear and structured way, especially how it affects multiple systems like the skin, eyes, and blood vessels, helping readers understand why early diagnosis and continuous care are so important. The way you connected symptoms, complications, and treatment options makes it easier for patients and families to recognize warning signs and seek timely medical support. A very informative and reassuring resource for anyone trying to better understand this complex autoimmune condition.