Introduction & Background of Brugada Syndrome
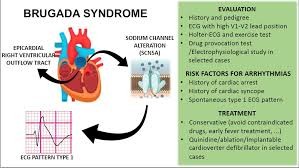
Brugada Syndrome (BrS) is a rare but potentially life-threatening genetic heart rhythm disorder (arrhythmia). It is characterized by a distinct abnormal pattern on an electrocardiogram (ECG), known as a Type 1 Brugada pattern, which shows a “coved” ST-segment elevation in the right precordial leads (V1-V2).
The primary mechanism involves a malfunction in the heart’s ion channels, most commonly the sodium channel. This defect disrupts the normal flow of sodium ions into the heart muscle cells, particularly in the right ventricle. This electrical instability can predispose individuals to dangerous ventricular arrhythmias, such as Ventricular Fibrillation (VF), which can cause the heart to stop pumping effectively. If not treated immediately, this leads to sudden cardiac arrest and, if untreated, increases the risk of sudden cardiac death.
BrS is a significant cause of sudden death in young, otherwise healthy adults, especially men of Asian descent, and is responsible for up to 20% of sudden deaths in individuals with structurally normal hearts.
Causes of Brugada Syndrome
Brugada Syndrome is primarily a genetic disorder, though not all cases have an identified genetic cause.
- Genetic Mutations: The most common known cause (in ~30% of cases) is a mutation in the SCN5A gene. This gene provides instructions for making a sodium channel that is critical for the heart’s electrical activity. Other, rarer gene mutations can also cause the syndrome.
- Inheritance Pattern: It is typically inherited in an autosomal dominant pattern, meaning a child only needs to inherit one copy of the defective gene from one parent to have the condition.
- Acquired Forms: In some cases, the characteristic Brugada ECG pattern can be unmasked or worsened by factors that affect ion channel function, such as:
- High fever
- Certain medications (sodium channel blockers, some antidepressants, anesthetics)
- Cocaine or alcohol abuse
- Electrolyte imbalances (e.g., high potassium, low potassium)
Indications of Brugada Syndrome
Indications are the signs or circumstances that point toward the presence of Brugada Syndrome.
- A Type 1 Brugada ECG pattern, either spontaneously or induced by a medication challenge test.
- A personal history of unexplained fainting (syncope), seizures, or cardiac arrest.
- A family history of Brugada Syndrome.
- A family history of sudden cardiac death before the age of 45.
- Nocturnal agonal respiration (gasping breaths during sleep).
Symptoms of Brugada Syndrome
Many people with Brugada Syndrome are asymptomatic and are only diagnosed after a routine ECG or a family member is diagnosed. When symptoms occur, they are directly related to the onset of a dangerous arrhythmia and include:
- Sudden Cardiac Arrest: The most severe symptom.
- Syncope (Fainting): Sudden loss of consciousness, often without warning.
- Palpitations: A feeling of a fast, fluttering, or pounding heartbeat.
- Seizures: Can occur due to lack of blood flow to the brain during an arrhythmia.
- Nocturnal Agonal Breathing: Gasping or gurgling sounds during sleep, which can be a sign of a nocturnal arrhythmia.
The presence of these symptoms, especially syncope, significantly increases the risk of sudden cardiac death.
Prevention Strategies of Brugada Syndrome
Since BrS is often genetic, prevention focuses on avoiding triggers and managing risk in diagnosed individuals.
- Family Screening: If one family member is diagnosed, all first-degree relatives (parents, siblings, children) should be evaluated with an ECG and possibly genetic testing.
- Avoiding Triggers:
- Fever Management: Treat fevers aggressively with antipyretics (e.g., acetaminophen, ibuprofen), as fever is a well-known trigger for arrhythmias in BrS.
- Medication Avoidance: Patients must avoid a long list of drugs known to aggravate the condition (see www.brugadadrugs.org for an updated list).
- Lifestyle Modifications:
- Avoid excessive alcohol consumption.
- Avoid illicit drug use, especially cocaine.
- Maintain a healthy electrolyte balance, especially during illness or exercise.
Myths and Facts About Brugada Syndrome
| Myth | Fact |
|---|---|
| Only older people get Brugada Syndrome. | It is most often diagnosed in adults aged 30-40, but it can affect children and the elderly. |
| If you have no symptoms, you are safe. | Asymptomatic individuals still have a significant, though lower, risk of sudden cardiac death. Risk stratification by a cardiologist is essential. |
| It’s a “man’s disease.” | While it is 8-10 times more common in men, women can also inherit and be affected by Brugada Syndrome. |
| An abnormal ECG alone means you need an ICD. | Not everyone with a Brugada ECG pattern needs an implantable cardioverter-defibrillator (ICD). The decision is based on overall risk (symptoms, ECG pattern). |
| Brugada Syndrome can be cured with medication. | There is no cure. Quinidine is used to reduce arrhythmia risk, but an ICD is the only proven therapy to terminate a life-threatening arrhythmia. |
Treatments and Therapy
The goal of treatment is to prevent sudden cardiac death by terminating or preventing dangerous ventricular arrhythmias.
Medication-Based Treatments
- Quinidine: An anti-arrhythmic drug that blocks specific potassium currents. It is used for patients at high risk, as a adjunct to an ICD, or for those with frequent ICD shocks. It can also be an option for asymptomatic patients with a spontaneous diagnostic ECG pattern.
Surgical Treatments
- Implantable Cardioverter-Defibrillator (ICD): This is the standard and most effective treatment for preventing sudden death in high-risk patients (those with a history of cardiac arrest or syncope). The device is implanted under the skin and continuously monitors the heartbeat. If a life-threatening arrhythmia is detected, it delivers an electric shock to restore a normal rhythm.
- Catheter Ablation: A relatively newer procedure where radiofrequency energy is used to destroy a small area of heart tissue in the right ventricle outflow tract that is thought to be the source of the arrhythmia. This can normalize the ECG and reduce arrhythmia events.
Lifestyle and Behavioral Interventions
- As outlined in the “Prevention Strategies” section, avoiding fever and specific medications is a critical behavioral intervention.
Physical Therapy and Rehabilitation
- Not a primary treatment for BrS itself. However, cardiac rehabilitation may be beneficial for patients after ICD implantation to help them safely resume physical activity and manage anxiety.
Alternative and Complementary Medicine
- No alternative therapies have been proven to treat the underlying ion channel defect or prevent sudden death. These should never replace standard medical care. Stress-reduction techniques like meditation may help with overall well-being but do not affect the arrhythmia risk.
Psychotherapy and Counseling
- Highly recommended. Living with a diagnosis that increases the risk of sudden cardiac death and managing an ICD can cause significant anxiety, depression, and fear. Psychological support is crucial for coping with the condition.
Immunizations and Vaccines
- No direct link, but staying up-to-date with vaccines (e.g., flu shot) can help prevent infections that lead to high fever, which is a known trigger.
Stem Cell Therapy & Gene Therapy
- These are currently experimental and not available as standard treatments. Research is ongoing to better understand the genetic basis and develop future targeted therapies, but they are not yet a clinical reality for BrS patients.
Top 20 FAQ with Answer on Brugada Syndrome
1. What is Brugada Syndrome?
It is a genetic heart disorder that causes a specific abnormal ECG pattern and can lead to dangerous fast heart rhythms, which increases the risk of sudden cardiac death.
2. How is it diagnosed?
Primarily through a 12-lead ECG showing a Type 1 Brugada pattern. If this pattern is not visible, a drug challenge test with sodium channel blockers may be used.
3. Is Brugada Syndrome hereditary?
Yes, in an autosomal dominant pattern. About 50-70% of families do not have an identified gene mutation.
4. Can it be cured?
There is no cure. Treatment focuses on managing the risk of sudden death.
5. What is the life expectancy?
With proper diagnosis and treatment (typically an ICD for high-risk patients), most individuals have a normal life expectancy.
6. Who is most at risk?
Symptomatic individuals (those with prior cardiac arrest or syncope) and those with a spontaneous Type 1 ECG pattern are at highest risk. Men are also at higher risk than women.
7. Can I exercise if I have Brugada Syndrome?
Moderate exercise is usually fine, but strenuous endurance athletics may be discouraged. You must discuss this with your cardiologist.
8. What medications should I avoid?
A wide range, including certain anti-arrhythmics, antidepressants, and anesthetics. Always consult www.brugadadrugs.org and inform all your doctors of your diagnosis.
9. Is it safe to get an anesthetic?
Yes, but it requires careful planning. You must inform your anesthesiologist about your diagnosis well before any surgery.
10. What should I do if I get a fever?
Treat it immediately with acetaminophen or ibuprofen and seek medical attention if it is high or persistent.
11. Can I drink alcohol?
Moderate consumption may be acceptable for some, but binge drinking is dangerous. Discuss with your doctor.
12. What is the main treatment?
For high-risk patients, an Implantable Cardioverter-Defibrillator (ICD) is the primary treatment to prevent sudden death.
13. Is an ICD always necessary?
No. For asymptomatic, low-risk patients, close monitoring and avoiding triggers may be sufficient.
14. Can children have Brugada Syndrome?
Yes, though it is less common. Family screening is crucial if a parent is diagnosed.
15. How does it cause sudden death?
By triggering a fast, chaotic heart rhythm called ventricular fibrillation, which stops the heart from pumping blood.
16. Are the symptoms constant?
No, the ECG pattern can fluctuate, and arrhythmias are episodic, often occurring at rest or during sleep.
17. Can stress trigger an event?
Emotional stress is a potential trigger for some individuals.
18. What’s the difference between Brugada Syndrome and a heart attack?
A heart attack is caused by a blocked artery damaging heart muscle. BrS is an electrical problem with no blockage.
19. Should my family get tested?
Yes, all first-degree relatives should be screened with an ECG.
20. Where can I find more information and support?
Reputable sources include the Heart Rhythm Society (HRS), BrugadaDrugs.org, and genetic counseling services.
Conclusion
Brugada Syndrome is a serious inherited cardiac condition that significantly increases the risk of sudden cardiac death in seemingly healthy individuals. While the diagnosis can be frightening, advancements in risk stratification and treatment, particularly the use of the ICD, have dramatically improved outcomes. A proactive approach involving accurate diagnosis, careful risk assessment, adherence to treatment plans, avoidance of known triggers, and psychological support is essential for managing the condition and allowing patients to live full, productive lives. Ongoing research continues to improve our understanding and management of this complex syndrome.
Find Trusted Cardiac Hospitals
Compare heart hospitals by city and services — all in one place.
Explore Hospitals
This article offers a clear and patient‑focused explanation of Brugada syndrome, helping readers understand how a genetic electrical heart disorder can increase the risk of dangerous arrhythmias and sudden cardiac events. The way it explains characteristic ECG patterns, common symptoms like fainting or palpitations, and risk stratification makes a complex cardiac condition more accessible for both patients and caregivers. I also appreciate the practical discussion of diagnosis, family screening, and treatment options like ICD placement, which empowers readers to engage in informed conversations with their healthcare providers. Overall, it’s an informative and well‑structured resource that raises awareness about this rare but serious heart condition.