Introduction & Background of Ehlers-Danlos Syndrome (Vascular Type) – Fragile skin and blood vessels
Ehlers-Danlos Syndrome (EDS) is a group of 13 heritable disorders that affect the body’s connective tissues—the proteins and other substances that provide support and structure to skin, bones, blood vessels, and other organs. The Vascular Type of EDS (vEDS), previously known as EDS type IV, is one of the most severe and life-threatening forms.
Its hallmark is a profound fragility of the blood vessels, hollow organs, and skin. This fragility stems from a genetic defect in the production or structure of Type III collagen, a critical protein that provides strength and elasticity to tissues like arteries, the uterus, and the intestines. Unlike other EDS types characterized by hypermobile joints and stretchy skin, vEDS presents with thin, translucent skin and a dramatically high risk of spontaneous arterial, intestinal, or uterine rupture. Managing vEDS requires a highly specialized, proactive, and cautious approach to prevent catastrophic complications.
Causes of Ehlers-Danlos Syndrome (Vascular Type)
vEDS is caused by a mutation in the COL3A1 gene. This gene provides the instructions for making the pro-alpha1(III) chain of Type III collagen.
- Inheritance: It is almost always inherited in an autosomal dominant pattern. This means only one copy of the mutated gene, inherited from either parent, is sufficient to cause the disorder. An affected parent has a 50% chance of passing the mutation to each child.
- De Novo Mutations: In approximately 50% of cases, there is no family history. The mutation occurs spontaneously (de novo) in the affected individual, who can then pass it on to their children.
Indications of Ehlers-Danlos Syndrome (Vascular Type)
Indications are the characteristic physical signs that alert clinicians to the possibility of vEDS.
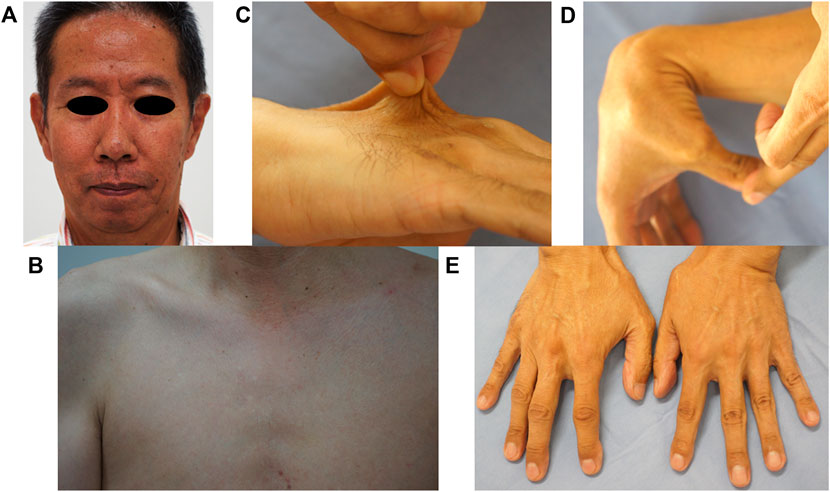
- Translucent Skin: The skin is often thin and pale, making the underlying venous network highly visible over the chest, abdomen, and limbs.
- Prominent Visible Veins: Extensive and easily visible veins are a key indicator.
- Characteristic Facial Features: Individuals may have a thin, pinched nose, thin lips, prominent eyes, and a lack of subcutaneous fat on the face, giving a “haunted” appearance.
- Easy Bruising: Severe and spontaneous bruising, often without significant trauma.
- Acrogeria: Prematurely aged appearance of the skin on the hands and feet.
Symptoms of Ehlers-Danlos Syndrome (Vascular Type)
Symptoms are the subjective experiences and major complications reported by the patient.
- Sudden, Severe Pain: This can indicate an arterial dissection (tear) or rupture. Common sites include the abdomen (mesenteric artery, renal artery) or chest (aortic dissection).
- Spontaneous Organ Rupture: The colon (large intestine) is the most common site for hollow organ rupture.
- Life-Threatening Bleeding: Arterial ruptures can lead to massive internal bleeding, shock, and death if not treated emergently.
- Complications of Pregnancy: Pregnant women with vEDS face a significantly high risk of uterine rupture during the third trimester or delivery.
- Pneumothorax: Collapsed lung (spontaneous pneumothorax).
- Joint Hypermobility: Typically limited to the small joints of the hands and feet.
Prevention Strategies of Ehlers-Danlos Syndrome (Vascular Type)
Prevention in vEDS focuses on avoiding complications, as the genetic condition itself cannot be prevented.
- Genetic Counseling & Testing: For individuals with a family history, genetic testing confirms the diagnosis and allows for informed family planning.
- Avoidance of Risky Activities: Contact sports, heavy lifting, and high-impact exercises are strictly discouraged.
- Medical Alert: Wearing a medical alert bracelet is crucial to inform emergency personnel of the condition in case of an accident.
- Medication Management:
- Avoid Anticoagulants and Antiplatelets: Drugs like warfarin, clopidogrel, and high-dose aspirin can increase bleeding risk and are generally contraindicated unless absolutely necessary.
- Celiprolol: This beta-blocker has been shown in studies to reduce the risk of arterial events in vEDS patients by reducing stress on the vessel walls.
- Conservative Surgical Approach: Any surgery or invasive procedure should be avoided unless life-saving. Techniques must be meticulous due to tissue fragility.
- Regular Monitoring: Non-invasive imaging (e.g., MRA or CT angiography) may be used to screen for arterial aneurysms or dissections, though the protocol is individualized.
Myths and Facts About Ehlers-Danlos Syndrome (Vascular Type)
| Myth | Fact |
|---|---|
| vEDS is just a “flexibility” disorder. | vEDS is a severe, life-threatening vascular disorder. While some joint hypermobility exists, the primary concern is fragile blood vessels and organs. |
| Everyone with EDS is at high risk of rupture. | The significant risk of spontaneous arterial or organ rupture is specific to the vascular type (vEDS), not the more common hypermobile type (hEDS). |
| A person with vEDS will definitely die young. | While vEDS reduces life expectancy, outcomes are highly variable. Proactive management, medication (like celiprolol), and lifestyle modifications are improving life expectancy and quality of life. |
| The skin is always stretchy in EDS. | In vEDS, the skin is not hyperelastic. It is thin, translucent, and fragile, tearing or bruising easily. |
| There is nothing that can be done. | While there is no cure, a great deal can be done. This includes preventive medication, emergency planning, genetic counseling, and specialized medical care to manage risks and complications. |
Treatments and Therapy for Ehlers-Danlos Syndrome (Vascular Type)
There is no cure for vEDS. Treatment is focused on managing symptoms, preventing complications, and responding to emergencies.
Medication-Based Treatments
- Celiprolol: A beta-blocker that is the first-line pharmacological therapy to reduce pulse pressure and stress on arterial walls, lowering the risk of arterial events.
- Pain Management: Careful use of pain medication for chronic pain, avoiding NSAIDs (e.g., ibuprofen, naproxen) due to their bleeding risk.
- Blood Pressure Control: Maintaining low-normal blood pressure to reduce stress on vessels.
Surgical Treatments
Surgery is high-risk and reserved for life-threatening situations.
- Endovascular Techniques: Preferred over open surgery when possible. Stent grafts can be used to repair aneurysms or dissections from within the vessel, causing less tissue trauma.
- Open Surgery: Requires a surgeon highly experienced in vEDS. Tissues are fragile and do not hold sutures well, leading to high rates of complications.
Physical Therapy and Rehabilitation
- Focuses on low-impact, safe exercises (e.g., swimming, walking) to maintain muscle tone and joint stability without raising blood pressure or causing trauma.
- Absolute avoidance of heavy lifting, weight training, contact sports, and manipulative techniques like chiropractic adjustment.
Lifestyle and Behavioral Interventions
- Diet: A healthy diet to maintain a healthy weight and avoid constipation, which can strain blood vessels.
- Smoking Cessation: Mandatory, as smoking dramatically increases the risk of vascular damage.
- Stress Management: Techniques like meditation to help control blood pressure.
Alternative and Complementary Medicine
- Gentle modalities like acupuncture (with caution due to bleeding risk) or mindfulness may help manage pain and stress.
- Always consult with the primary vEDS care team before starting any alternative therapy.
Psychotherapy and Counseling
- Essential for coping with the anxiety, depression, and psychological burden of living with a chronic, life-threatening condition.
- Genetic counseling is a critical component for the patient and their family.
Immunizations and Vaccines
- Standard vaccinations are encouraged to prevent infections that could cause stress on the body.
- The COVID-19 vaccine is particularly important, as the virus itself can cause vascular inflammation and clotting issues.
Stem Cell Therapy
- Currently, this is not a treatment for vEDS and is considered purely experimental within the context of clinical research.
Gene Therapy
- Gene therapy is a long-term goal and area of active research but is not currently available or proven for vEDS. The concept is to deliver a functional copy of the COL3A1 gene to correct the underlying defect.
Top 20 FAQ with Answer on Ehlers-Danlos Syndrome (Vascular Type)
1. What is the life expectancy for someone with vEDS?
While reduced, life expectancy has improved with modern management. The median life expectancy is now often cited as around 50 years, but this varies widely. Many live longer with careful care.
2. Can you have mild vEDS?
vEDS is a serious condition by definition. However, the age of first major complication and the frequency of events can vary significantly between individuals, even within the same family.
3. How is vEDS diagnosed?
Diagnosis is confirmed through genetic testing identifying a mutation in the COL3A1 gene. Clinical evaluation (skin, facial features, history) guides who should be tested.
4. What is the difference between vEDS and other types of EDS?
The key difference is the primary site of involvement: vEDS primarily affects blood vessels and hollow organs, while hEDS primarily affects joints, and classical EDS primarily affects the skin.
5. Is vEDS contagious?
No. It is an inherited genetic disorder.
6. Can women with vEDS have children?
Pregnancy is considered very high-risk for both mother and fetus. There is a significant risk of uterine rupture and arterial dissection. It requires extensive pre-conception counseling with a high-risk obstetric team and a medical geneticist.
7. What should I do in a medical emergency?
Go to the nearest emergency room immediately. Inform staff of your vEDS diagnosis and show your medical alert bracelet. Sudden, severe pain in the abdomen or chest is a medical emergency.
8. What medications should be avoided?
Avoid blood thinners (warfarin, clopidogrel), high-dose aspirin, and NSAIDs (ibuprofen, naproxen) due to bleeding risk. Always discuss medications with a vEDS-knowledgeable doctor.
9. Can I exercise?
Yes, but carefully. Low-impact activities like walking, swimming, and stationary biking are best. Avoid heavy lifting, sprinting, contact sports, and anything that raises blood pressure significantly.
10. Is it safe to see a chiropractor?
No. Spinal manipulation poses a high risk of causing arterial dissection (e.g., vertebral or carotid artery) and is absolutely contraindicated.
11. Why is my skin so thin and see-through?
The lack of sufficient, strong Type III collagen results in thinner skin layers and less underlying fat, making the veins underneath highly visible.
12. Can vEDS be detected before birth?
Yes, through prenatal genetic testing such as chorionic villus sampling (CVS) or amniocentesis if the familial COL3A1 mutation is known.
13. What kind of doctor manages vEDS?
Care is typically coordinated by a medical geneticist or a vascular specialist with experience in connective tissue disorders, alongside a multidisciplinary team (cardiologist, surgeon, etc.).
14. Does celiprolol cure vEDS?
No. It is a preventive medication that has been shown to reduce the rate of arterial events, but it does not correct the underlying collagen defect.
15. Why do I bruise so easily?
The fragile blood vessels and thin skin mean that even minor trauma can cause capillaries to break and bleed into the surrounding tissue.
16. Are there any new treatments on the horizon?
Research is ongoing, particularly in the areas of gene therapy and drugs that can help “chaperone” misfolded collagen proteins to function better.
17. Can a person with vEDS donate blood?
Typically, no. The vascular fragility and potential for complications make them unsuitable donors.
18. How does vEDS affect the eyes?
The sclera (white of the eye) can appear blueish due to its thinness, allowing the underlying dark layer to show through. There is also an increased risk of retinal detachment.
19. Is it safe to have dental work?
Yes, but inform your dentist of your diagnosis. They may need to take extra care due to a potential for easy bleeding and fragile oral tissues.
20. Where can I find support?
Organizations like The Ehlers-Danlos Society (ehlers-danlos.com) provide invaluable resources, support networks, and information for patients and families.
Conclusion
Ehlers-Danlos Syndrome, Vascular Type, is a profound and challenging genetic condition that demands respect and a highly specialized approach to care. Its defining feature—the fragility of blood vessels and organs—poses a constant threat, but it is not a hopeless diagnosis. Through accurate genetic diagnosis, proactive medical management with medications like celiprolol, strict lifestyle adaptations, and comprehensive emergency planning, individuals with vEDS can significantly mitigate their risks. Ongoing research provides hope for future therapies. The cornerstone of living with vEDS is education, a strong partnership with a knowledgeable medical team, and a vigilant, yet empowered, approach to health.
Find Trusted Cardiac Hospitals
Compare heart hospitals by city and services — all in one place.
Explore Hospitals
This clinical guide explains Vascular Ehlers-Danlos Syndrome with impressive clarity, especially how it connects genetic factors with serious vascular risks and the importance of early monitoring. I appreciated the focus on recognizing warning signs, preventive care, and careful long-term management, which makes the content both informative and reassuring for readers. Well-structured, compassionate, and very helpful for raising awareness about this rare but critical condition