Introduction & Background of Kawasaki Disease
Kawasaki Disease (KD), also known as mucocutaneous lymph node syndrome, is an acute illness characterized by inflammation of the blood vessels throughout the body (vasculitis). It primarily affects infants and young children under the age of 5, with a peak incidence in toddlers. First described in 1967 by the Japanese pediatrician Dr. Tomisaku Kawasaki, its exact cause remains unknown, but it is now the leading cause of acquired heart disease in children in developed countries.
The inflammation predominantly targets the coronary arteries, which supply oxygen-rich blood to the heart muscle. If not diagnosed and treated promptly, this can lead to the formation of coronary artery aneurysms (weakened, bulging sections of the artery wall), which can increase the risk of heart attacks, heart failure, or sudden death later in life. Early intervention is critical to reduce this risk significantly.
Causes of Kawasaki Disease
The precise cause of Kawasaki Disease is unknown. The prevailing scientific theory is that it is triggered by an infectious agent (like a virus or bacteria) in genetically susceptible children. This suggests it is not directly contagious from person to person.
- Infectious Trigger: The symptoms (fever, rash, swollen glands) resemble an infection, and the disease often occurs in seasonal outbreaks, pointing to a widespread but unidentified pathogen.
- Genetic Predisposition: KD is more common in children of Asian descent (especially Japanese and Korean), even when they live in other parts of the world. Certain genes related to immune system function are believed to increase a child’s susceptibility.
- Immune System Response: The leading hypothesis is that an unknown trigger causes the immune system to mount an abnormal, intense inflammatory response that mistakenly attacks the body’s own blood vessels.
Indications of Kawasaki Disease
“Indications” in a medical context often refer to reasons for a treatment or a sign that a condition is present. For Kawasaki Disease, the primary indication is the presence of a specific set of clinical criteria. A doctor will strongly suspect KD in a child who has:
- A persistent high fever (≥102.2°F or 39°C) for at least 5 days.
- Plus, at least four of the following five principal clinical features:
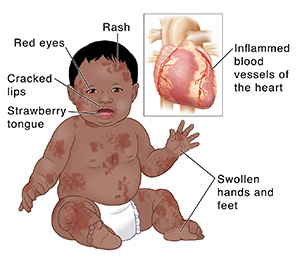
Symptoms of Kawasaki Disease
The symptoms of KD occur in phases.
Phase 1: Acute Febrile Phase (Weeks 1-2)
- High Fever: The hallmark symptom; often spiking to 104°F (40°C) and not responsive to typical antibiotics or antipyretics. Lasts an average of 1-2 weeks.
- Rash: A widespread, non-specific rash, often in the diaper area or on the trunk.
- Extremity Changes:
- Redness: Reddened palms of the hands and soles of the feet.
- Swelling: Swollen hands and feet.
- Peeling: Later in the illness (around week 2 or 3), skin on the fingers and toes may begin to peel in sheets.
- Conjunctival Injection: Redness in both eyes (bilateral conjunctivitis) without pus or discharge.
- Changes in Lips and Mouth:
- Cracked, red, swollen lips.
- “Strawberry Tongue,” where the tongue is red, bumpy, and coated.
- Redness inside the mouth and the back of the throat.
- Swollen Lymph Nodes: A single, large, swollen lymph node in the neck (larger than 1.5 cm), often only on one side.
Phase 2: Subacute Phase (Weeks 2-4)
The fever, rash, and swollen glands usually resolve, but the child may remain irritable. This is the critical period when coronary artery aneurysms may develop. Peeling of the fingers and toes is common at the start of this phase.
Phase 3: Convalescent Phase (Weeks 4+)
Symptoms gradually disappear, and blood tests return to normal. This phase can last until all signs of inflammation have resolved, which may take several months.
Prevention Strategies of Kawasaki Disease
Since the cause is unknown, there are no known ways to prevent Kawasaki Disease. The most crucial strategy is early recognition and treatment to prevent cardiac complications. Parents and caregivers should be aware of the symptoms and seek immediate medical attention if they suspect KD.
Myths and Facts About Kawasaki Disease
| Myth | Fact |
|---|---|
| KD is contagious. | It is not considered contagious. It does not spread between children in households or daycare centers. |
| Only Asian children get it. | While children of Asian and Pacific Island descent are at highest risk, KD can affect children of any racial or ethnic background. |
| It’s just a bad fever and rash. | It is a serious illness that can cause lifelong heart damage if not treated promptly. |
| If the fever goes away, the child is fine. | The most dangerous phase for the heart can occur after the fever breaks. Follow-up care is essential. |
| There is a cure for KD. | There is no “cure,” but highly effective treatments exist to reduce inflammation and prevent heart damage. |
Treatments and Therapy
The primary goal of treatment is to reduce inflammation in the blood vessels, prevent coronary artery damage, and manage symptoms.
Medication-Based Treatments
- Intravenous Immunoglobulin (IVIG): This is the cornerstone of treatment. It is a blood product containing antibodies given as a single, high-dose infusion. It is most effective when administered within the first 10 days of the illness and significantly reduces the risk of coronary artery aneurysms.
- Aspirin: High-dose aspirin is used during the acute phase for its potent anti-inflammatory and anti-platelet effects. Once the fever resolves, a low dose is continued for its blood-thinning (anti-platelet) properties to prevent blood clots, especially in children who develop coronary artery changes.
Surgical Treatments
Surgery is only necessary for the small percentage of children who develop significant coronary artery complications.
- Coronary Artery Bypass Grafting (CABG): To bypass blocked coronary arteries.
- Percutaneous Coronary Intervention (PCI): Such as balloon angioplasty or stent placement, to open narrowed arteries.
- Heart Transplant: In extremely rare cases of severe, irreversible damage to the heart muscle.
Physical Therapy and Rehabilitation
Not typically a standard part of KD treatment unless the child has suffered a stroke or other neurological complication due to blood clots, in which case rehab would be necessary.
Lifestyle and Behavioral Interventions
Long-term management focuses on heart-healthy living:
- A balanced, low-fat diet.
- Regular physical activity as approved by a cardiologist.
- Avoiding smoking and secondhand smoke.
- Maintaining a healthy weight.
Alternative and Complementary Medicine
There is no proven alternative therapy to replace IVIG and aspirin. These should never be used as a substitute for standard medical care.
Psychotherapy and Counseling
A KD diagnosis can be stressful for the child and family. Counseling can help manage anxiety, especially related to long-term cardiac risks and the challenges of a prolonged illness.
Immunizations and Vaccines
Important: Live-virus vaccines (like MMR and Varicella) must be delayed for 11 months after IVIG treatment, as IVIG can interfere with the body’s immune response to the vaccine.
Stem Cell Therapy
This is not a standard or approved treatment for Kawasaki Disease and is considered purely experimental.
Gene Therapy
This is not a current treatment for KD. Research is focused on identifying genetic markers of susceptibility, not on gene-based interventions.
Top 20 FAQ with Answers on Kawasaki Disease
- What is Kawasaki Disease?
It is an acute illness causing inflammation of blood vessels (vasculitis) primarily in young children, which can lead to heart complications. - What causes it?
The cause is unknown, but it is likely an abnormal immune response to an unknown infection in genetically predisposed children. - Is it contagious?
No, it is not considered contagious. - What age group does it affect?
Over 80% of cases are in children under 5, with the peak incidence between 1 and 2 years old. - What are the classic symptoms?
A high fever for 5+ days, plus at least four of: rash, red eyes, changes in lips/mouth, swollen hands/feet, and a swollen lymph node. - How is it diagnosed?
There is no single test. Diagnosis is based on the clinical symptoms and supported by blood tests and an echocardiogram (heart ultrasound). - How is it treated?
With a single infusion of Intravenous Immunoglobulin (IVIG) and high-dose aspirin. - What are the potential complications?
The most serious complication is the development of coronary artery aneurysms, which can lead to heart attacks or heart rhythm problems. - Can it be fatal?
Yes, but with timely diagnosis and treatment, the mortality rate is very low (less than 0.5% in the U.S.). - Does it have long-term effects?
Children without coronary artery changes typically recover fully. Those with aneurysms require lifelong cardiology follow-up. - Will my child need heart surgery?
Only a small minority of children (less than 5% with treatment) develop aneurysms large enough to potentially require surgery. - Can you get Kawasaki Disease twice?
Recurrence is rare but possible, occurring in about 1-3% of cases. - What is the follow-up care?
All children need an echocardiogram at diagnosis and again at 6-8 weeks. Those with normal arteries may be discharged. Those with abnormalities need ongoing monitoring. - Is there a link to COVID-19?
Yes. A condition called Multisystem Inflammatory Syndrome in Children (MIS-C) shares some features with KD and is linked to COVID-19 infection. However, it is considered a distinct illness. - Why is aspirin used in children?
Aspirin is usually avoided in children due to Reye’s syndrome risk. However, under a doctor’s supervision for KD, the benefits of preventing blood clots outweigh this small risk. - Can adults get Kawasaki Disease?
It is exceedingly rare in adults. When it occurs, it is often called “Kawasaki-like” illness. - Does it run in families?
While not directly hereditary, having a sibling who had KD slightly increases the risk, suggesting a genetic component. - What should I do if I suspect my child has it?
Contact your pediatrician or go to the emergency room immediately. Emphasize the persistent high fever and the other symptoms. - What is the “peeling” phase?
Around the second week of illness, the skin on the fingers and toes may peel off in large sheets. This is a classic sign during the recovery phase. - Can my child live a normal life after KD?
Absolutely. The vast majority of children with KD who receive timely treatment go on to live completely normal, healthy lives without any cardiac sequelae.
Conclusion
Kawasaki Disease is a formidable but manageable childhood illness. Its mystery lies in its unknown cause, but its power to cause harm has been greatly diminished by modern medical treatment. The key to a positive outcome is awareness and swift action. Recognizing the distinctive constellation of symptoms—a persistent high fever accompanied by specific physical signs—and seeking immediate medical care can ensure a child receives the life-saving treatment of IVIG and aspirin, dramatically reducing the risk of long-term heart damage. Through continued research, vigilant clinical care, and informed parents, the threat of Kawasaki Disease can be effectively neutralized, allowing affected children to thrive.
Find Trusted Cardiac Hospitals
Compare heart hospitals by city and services — all in one place.
Explore Hospitals
This article does a great job breaking down Kawasaki disease in a way that’s easy for parents and caregivers to understand, especially how the inflammation of blood vessels primarily affects young children. The explanation of common symptoms like prolonged fever, rash, and swollen hands and feet helps readers recognize warning signs early, which is so important for timely treatment. I also appreciate the clear discussion of diagnostic criteria, possible complications like heart involvement, and the importance of therapies that reduce inflammation. Overall, it’s an informative and reassuring guide that raises awareness about this condition and supports proactive care.