Introduction & Background of Menkes Disease
Menkes Disease, also known as Menkes syndrome or kinky hair disease, is a rare, severe, and often fatal X-linked recessive genetic disorder that affects copper levels in the body. It is characterized by a cellular copper transport deficiency, leading to a functional copper deficiency despite adequate dietary intake.
The core problem lies not in the absorption of copper from the gut but in its distribution throughout the body. In a healthy individual, copper absorbed by the intestines is transported to the liver and then distributed to various enzymes and tissues that require it. In Menkes Disease, a mutation in the ATP7A gene disrupts this process. This gene is responsible for producing a protein that transports copper across cellular membranes, including the intestinal lining and the blood-brain barrier. Consequently, copper accumulates in certain tissues like the intestine and kidneys while being deficient in the brain, blood, and other vital areas. This systemic copper deficiency impairs the function of numerous copper-dependent enzymes, leading to the widespread symptoms of the disease.
Causes of Menkes Disease
The primary cause of Menkes Disease is a mutation in the ATP7A gene located on the X chromosome (Xq21.1).
- Inheritance Pattern: X-linked recessive. This means:
- The gene is on the X chromosome.
- Males (who have one X and one Y chromosome) are primarily affected. If their single X chromosome has the mutation, they will have the disease.
- Females (who have two X chromosomes) can be carriers. They typically do not show symptoms because the healthy X chromosome can compensate, though some may exhibit mild symptoms.
- An affected male will pass his Y chromosome to all his sons (who will be unaffected) and his mutated X chromosome to all his daughters (who will be carriers).
- A female carrier has a 50% chance of passing the mutated X chromosome to a son (who would be affected) and a 50% chance of passing it to a daughter (who would be a carrier).
Indications of Menkes Disease
The initial indications often appear in the neonatal period or early infancy. Key early signs include:
- Poor Feeding and Failure to Thrive: Difficulty sucking, vomiting, and poor weight gain.
- Hypotonia: Profound floppiness and muscle weakness (low muscle tone).
- Hypothermia: Low body temperature.
- Neurological Deterioration: Developmental delay and seizures.
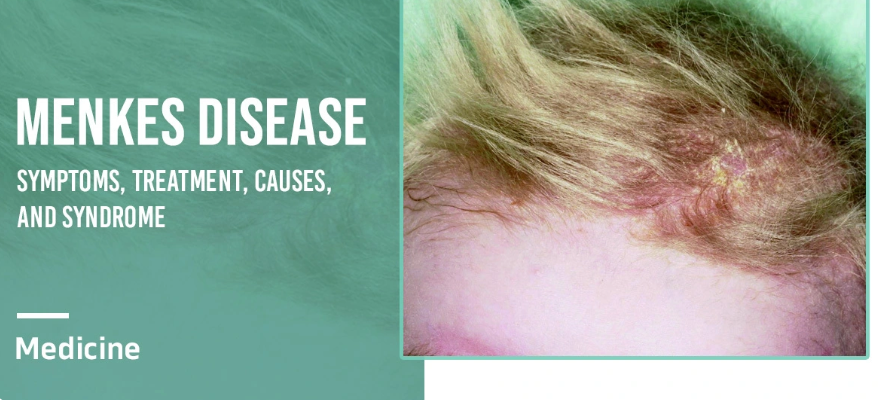
- Characteristic Hair: The hair is often sparse, coarse, brittle, and lightly pigmented, appearing “steely” or “kinky” under a microscope (pili torti).
Symptoms of Menkes Disease
As the disease progresses, a wide range of symptoms develops due to the failure of copper-dependent enzymes:
- Neurological: Seizures, severe intellectual disability, developmental regression, and neurodegeneration.
- Musculoskeletal: Hypotonia, weakness, joint laxity, and osteoporosis leading to frequent fractures.
- Cutaneous: The distinctive kinky hair, as well as pale, lax, and saggy skin, particularly on the trunk and neck.
- Vascular: Abnormalities in blood vessels, including tortuous (twisted) and fragile arteries, which can lead to internal bleeding or strokes.
- Facial Features: Some infants have a “cherubic” appearance with pudgy cheeks, a sagging face, and a depressed nasal bridge.
- Autonomic Dysfunction: Temperature instability and hypoglycemia.
- Gastrointestinal: Feeding difficulties, gastroesophageal reflux, and diarrhea.
Prevention Strategies
As a genetic disorder, Menkes Disease cannot be prevented in the traditional sense. However, proactive strategies can help in managing risk and outcomes:
- Genetic Counseling: For families with a known history of Menkes Disease or where a female is identified as a carrier. This helps understand the risks of passing the disease to children.
- Prenatal Testing: If there is a known family history, prenatal diagnosis is available through:
- Chorionic Villus Sampling (CVS): Performed at 10-13 weeks.
- Amniocentesis: Performed at 15-20 weeks.
These tests can analyze fetal DNA for mutations in the ATP7A gene.
- Newborn Screening and Early Diagnosis: While not yet universal, research is ongoing to develop newborn screening tests. Early diagnosis, ideally before symptoms appear, is critical for improving outcomes with early treatment.
Myths and Facts About Menkes Disease
| Myth | Fact |
|---|---|
| It’s caused by a lack of copper in the diet. | It is caused by a genetic defect that prevents the body from using copper properly, not a dietary deficiency. |
| It only affects boys. | Primarily, yes, but female carriers can sometimes exhibit mild symptoms, such as patchy hair abnormalities or learning difficulties. |
| Supplementing with high-dose copper can cure it. | Copper injections (see Treatment) can help if started very early, but they are not a cure. They manage symptoms and can improve outcomes. |
| Children with Menkes cannot interact at all. | While severely affected, these children can often interact with their caregivers, respond to voices and touch, and benefit from a loving, stimulating environment. |
Treatments and Therapy
There is no cure for Menkes Disease. Treatment focuses on early intervention to correct the copper deficiency and manage symptoms.
Medication-Based Treatments
- Copper Histidinate Injections: This is the primary treatment. It involves daily subcutaneous (under the skin) injections of copper-histidinate, a form of copper that can bypass the defective intestinal transport system and enter the bloodstream. The success of this treatment is highly dependent on starting it as early as possible, ideally within the first few weeks of life.
Surgical Treatments
- Surgery may be required to manage complications, such as inserting a gastrostomy tube (G-tube) for safe feeding or correcting certain vascular abnormalities.
Physical Therapy and Rehabilitation
- Essential for maintaining joint mobility, preventing contractures, managing muscle tone, and maximizing the child’s physical potential.
Lifestyle and Behavioral Interventions
- Nutritional Support: Working with a dietitian to ensure adequate calorie intake, often via a G-tube.
- Seizure Management: Creating a safe environment and adhering strictly to anti-epileptic medication schedules.
- Comfort Care: Focus on pain management, managing reflux, and ensuring overall comfort and quality of life.
Alternative and Complementary Medicine
- These are not substitutes for copper treatment. Some families may explore therapies like massage for comfort or music therapy for sensory stimulation, which should be discussed with the primary medical team.
Psychotherapy and Counseling
- Crucial for parents and family members to cope with the emotional stress, grief, and challenges of caring for a child with a progressive, life-limiting illness.
Immunizations and Vaccines
- Children with Menkes should receive all standard childhood vaccinations unless specifically contraindicated by their neurologist (e.g., in cases of severe seizures).
Stem Cell Therapy
- Still considered experimental. The theory is that stem cells could potentially produce the missing ATP7A protein, but it is not a standard treatment and has shown limited success.
Gene Therapy
- An area of active research. The goal is to introduce a functional copy of the ATP7A gene into the patient’s cells to correct the underlying genetic defect. While promising, it is not yet available as a clinical treatment.
Top 20 FAQ with Answer on Menkes Disease
1. What is the life expectancy for a child with Menkes Disease?
Unfortunately, the prognosis is often poor. Most children with the classic, severe form of Menkes disease do not survive beyond the first 3-10 years of life. Milder forms (like Occipital Horn Syndrome) are associated with a longer lifespan.
2. Is Menkes Disease curable?
No, there is currently no cure. Treatment aims to manage symptoms and improve quality of life.
3. Can girls get Menkes Disease?
It is extremely rare. Girls have two X chromosomes, so a mutation on one X is usually compensated for by the other. They are typically carriers but can rarely exhibit symptoms if the X-inactivation is skewed.
4. How is Menkes Disease diagnosed?
Diagnosis involves clinical evaluation, identification of low copper and ceruloplasmin levels in the blood, and confirmation through genetic testing identifying a mutation in the ATP7A gene.
5. What is the “kinky hair” in Menkes Disease?
The hair is twisted (a condition called pili torti), sparse, brittle, and lacks pigment, giving it a steely or kinky appearance. It is a classic diagnostic clue.
6. When do symptoms of Menkes first appear?
Symptoms typically begin within the first 2-3 months of life.
7. What is the main treatment for Menkes?
The primary treatment is early administration of daily subcutaneous copper histidinate injections.
8. Why does early treatment with copper matter?
Starting copper injections before significant neurological damage occurs (ideally in the first 4-6 weeks) offers the best chance for improved neurodevelopmental outcomes.
9. Is Menkes Disease contagious?
No, it is a genetic disorder and cannot be spread from person to person.
10. Can it be detected during pregnancy?
Yes, through prenatal genetic testing like CVS or amniocentesis if there is a known family history.
11. What is the difference between Menkes and Wilson’s Disease?
They are opposites. Menkes is a copper deficiency disorder due to poor transport. Wilson’s is a copper toxicity disorder due to the body’s inability to excrete excess copper.
12. Do oral copper supplements work?
No, because the defect is in intestinal absorption. Oral copper cannot be absorbed properly and will not reach the tissues that need it.
13. What are the chances of having another child with Menkes?
For a carrier mother, there is a 25% chance with each pregnancy of having an affected son and a 25% chance of having a carrier daughter.
14. Are there any support groups for families?
Yes, organizations like the Menkes Foundation and the NIH’s Genetic and Rare Diseases (GARD) Information Center provide resources and support.
15. What causes the neurological problems?
The brain is severely deprived of copper, which is a cofactor for enzymes critical for brain development, neurotransmitter production, and antioxidant defense.
16. Is there a milder form of Menkes?
Yes, variants like Mild Menkes or Occipital Horn Syndrome exist, with later onset and less severe symptoms, primarily affecting connective tissue.
17. What is the role of a feeding tube (G-tube)?
Many children have severe feeding difficulties and aspiration risk. A G-tube ensures safe and adequate nutrition and hydration.
18. Can physical therapy help?
Yes, it is vital for maintaining range of motion, managing muscle tone, and preventing complications like joint contractures.
19. What research is being done?
Research is focused on improving copper delivery methods, developing newborn screening protocols, and advancing gene therapy as a potential future cure.
20. How can I be tested to see if I’m a carrier?
If a mutation is known in the family, a female relative can undergo genetic testing to determine her carrier status.
Conclusion
Menkes Disease is a devastating genetic disorder that underscores the critical importance of trace metals in human development. While the prognosis for the classic form remains severe, significant strides have been made in understanding its molecular basis. The emphasis on early diagnosis through increased awareness and the potential for newborn screening, coupled with the standard of care—early copper histidinate injection—offers a beacon of hope for improving outcomes. Ongoing research into advanced therapies like gene therapy continues to fuel the quest for a future cure, while current multidisciplinary care focuses on maximizing the quality of life for affected children and providing crucial support for their families.
Find Trusted Cardiac Hospitals
Compare heart hospitals by city and services — all in one place.
Explore Hospitals
Here’s one useful, knowledgeable paragraph comment you can use for that blog:
This is a highly informative and well-structured guide on Menkes disease, especially for readers who may not be familiar with rare genetic metabolic disorders. The explanation of copper transport dysfunction, early symptoms such as developmental delays and hair abnormalities, and the importance of early diagnosis provides strong educational value for both healthcare professionals and general audiences. I also appreciate how the article highlights treatment approaches, supportive care strategies, and the role of genetic testing in confirming the condition. Content like this helps raise awareness about rare pediatric disorders and encourages early medical consultation, which can significantly impact patient outcomes and long-term quality of life.