Introduction & Background of Myasthenia Gravis – Weakness in Voluntary Muscles
Myasthenia Gravis (MG) is a chronic autoimmune neuromuscular disorder characterized by varying degrees of weakness in the voluntary muscles. The name is Latin and Greek for “grave muscular weakness,” but with modern treatments, the prognosis is generally good, and most individuals can lead full lives.
The core problem in MG is a breakdown in normal communication between nerves and muscles. At the neuromuscular junction (the point where nerve cells connect with the muscles they control), the body’s own immune system mistakenly produces antibodies that attack and destroy or block receptors for acetylcholine (ACh). ACh is the primary chemical neurotransmitter that signals muscles to contract. With fewer functional receptors, the muscles receive fewer nerve signals, leading to muscle weakness and rapid fatigue.
Causes of Myasthenia Gravis
MG is an autoimmune disorder, meaning the immune system, which normally protects the body from foreign invaders, mistakenly attacks its own tissues. The specific causes are not fully understood, but it is believed to be a combination of factors:
- Autoantibodies: In about 85% of MG patients, antibodies target the acetylcholine receptors (AChR) on the muscle side of the neuromuscular junction. Another subset of patients has antibodies against a muscle-specific kinase (MuSK), which is involved in organizing ACh receptors.
- Thymus Gland Abnormalities: The thymus gland, part of the immune system located in the upper chest, is often abnormal in MG patients. About 15% of MG patients have a thymoma (a tumor of the thymus, usually benign). In others, the thymus is enlarged (hyperplastic). The thymus is thought to play a key role in initiating the autoimmune response.
- Genetic Predisposition: While not directly inherited, there may be a genetic susceptibility that makes some individuals more prone to developing autoimmune disorders.
- Triggers: In genetically susceptible individuals, factors like infections, surgery, or stress may trigger the onset of the disease.
Indications of Myasthenia Gravis
“Indications” often refer to the signs that lead a doctor to suspect the condition. The primary indication of MG is fluctuating muscle weakness that worsens with activity and improves with rest. Key indicators include:
- Weakness that is typically worse later in the day.
- Symptoms that improve after cooling or resting.
- A specific pattern of muscle involvement (e.g., eyes, face, throat, and neck before limbs).
Symptoms of Myasthenia Gravis
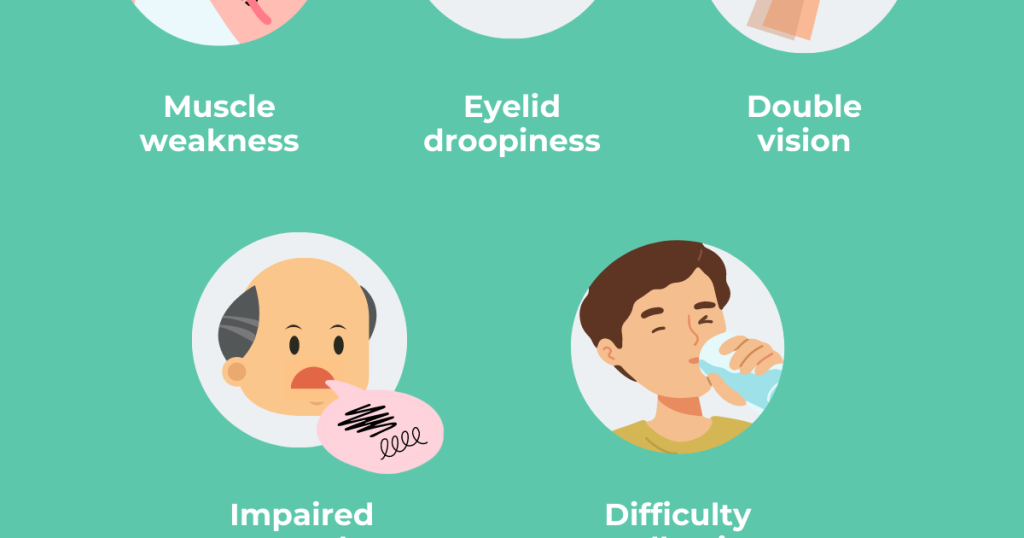
The symptoms can vary greatly in type and severity:
- Ocular Weakness: Drooping of one or both eyelids (ptosis), double vision (diplopia).
- Facial and Throat Muscle Weakness: Impaired speech (dysarthria), which may sound soft or nasal; difficulty swallowing (dysphagia), leading to choking on saliva, liquids, or food; changes in facial expression.
- Limb Weakness: Weakness in the arms, hands, fingers, legs, and neck. This can make it hard to hold arms up, grip objects, walk, or hold up the head.
- Respiratory Muscle Weakness: This is the most serious symptom and can lead to a “myasthenic crisis,” a life-threatening condition where breathing becomes insufficient, requiring emergency ventilation.
Prevention Strategies of Myasthenia Gravis
As an autoimmune disorder with no known direct cause, MG cannot be prevented. However, individuals diagnosed with MG can prevent exacerbations (worsening of symptoms) and complications by:
- Avoiding Triggers: Such as infections, stress, extreme heat, and overexertion.
- Medication Caution: Informing all doctors of their MG diagnosis, as many common medications (e.g., certain antibiotics, beta-blockers, anesthetics) can worsen symptoms.
- Sticking to Treatment Plans: Adhering to medication schedules and follow-up appointments.
- Getting Vaccinated: Preventing illnesses like flu and pneumonia can reduce the risk of an MG flare-up triggered by infection.
Myths and Facts About Myasthenia Gravis
| Myth | Fact |
|---|---|
| MG is a form of muscular dystrophy. | MG is an autoimmune disorder, not a degenerative muscle disease. The muscle tissue itself is healthy. |
| MG is contagious. | It is an autoimmune condition and cannot be spread from person to person. |
| Everyone with MG ends up in a wheelchair. | With proper treatment, most people with MG can lead active, normal or near-normal lives. |
| Weakness is constant and unchangeable. | Weakness in MG is highly variable and fluctuates, often improving with rest. |
| MG is a psychological condition. | MG is a very real and well-understood physical/physiological disorder. |
| Women with MG cannot have children. | With careful management by a healthcare team, most women can have successful pregnancies. |
Treatments and Therapy
MG treatment aims to improve muscle strength and suppress the autoimmune response.
Medication-Based Treatments
- Cholinesterase Inhibitors: Drugs like pyridostigmine (Mestinon) improve communication between nerves and muscles by slowing the breakdown of acetylcholine, providing temporary symptom relief.
- Immunosuppressants: Corticosteroids (e.g., prednisone) and other agents (e.g., azathioprine, mycophenolate mofetil) suppress the abnormal immune system activity over the long term.
Surgical Treatments
- Thymectomy: Surgical removal of the thymus gland. This can reduce symptoms and may lead to remission, especially in patients with thymoma or early-onset AChR-positive MG.
Physical Therapy and Rehabilitation
- Focuses on maintaining muscle strength and overall fitness without causing excessive fatigue. A therapist can design a safe, low-impact exercise program.
Lifestyle and Behavioral Interventions
- Energy Conservation: Pacing activities, taking frequent rests, and using adaptive devices.
- Dietary Modifications: Eating soft foods or smaller, more frequent meals if swallowing is difficult.
- Stress Management: Techniques like meditation and yoga can help manage stress, a known trigger.
Alternative and Complementary Medicine
- While not a substitute for standard care, some patients find acupuncture, massage, or certain supplements helpful for managing stress and mild discomfort. Always consult a doctor before starting any complementary therapy.
Psychotherapy and Counseling
- Living with a chronic illness can be challenging. Counseling can help manage anxiety, depression, and the emotional impact of the diagnosis.
Immunizations and Vaccines
- Staying up-to-date on vaccinations (especially for flu and pneumonia) is crucial to prevent infections that can trigger a crisis. However, live vaccines may not be safe for those on strong immunosuppressants.
Stem Cell Therapy
- This is an experimental treatment that aims to “reboot” the immune system. It is not a standard therapy for MG and is only available in clinical trials for severe, treatment-resistant cases.
Gene Therapy
- Gene therapy for MG is still in the early research stage and is not available as a treatment. It explores ways to correct the underlying immune dysregulation.
Top 20 FAQ with Answers on Myasthenia Gravis
1. Is Myasthenia Gravis fatal?
While a myasthenic crisis (severe breathing difficulty) can be life-threatening, with modern treatments and management, the vast majority of patients have a normal life expectancy and a good quality of life.
2. Is MG contagious or inherited?
No, MG is not contagious. It is rarely inherited, though a genetic predisposition to autoimmune disorders may exist in some families.
3. What is the life expectancy for someone with MG?
With current treatments, life expectancy for people with MG is typically normal.
4. Can MG go into remission?
Yes, some patients can achieve remission, where symptoms disappear completely or significantly, either temporarily or permanently, especially after treatments like thymectomy.
5. What triggers an MG flare-up?
Common triggers include infection, stress, surgery, extreme heat, lack of sleep, and certain medications.
6. What medications should MG patients avoid?
Many, including certain antibiotics (e.g., fluoroquinolones, macrolides), beta-blockers, magnesium, and some anesthetics. Always provide your doctor with a complete list of your medications.
7. Can women with MG have a healthy pregnancy?
Yes, but it requires careful planning and management by a high-risk obstetrician and neurologist. Symptoms can fluctuate during and after pregnancy.
8. Is exercise recommended for MG patients?
Yes, but it must be carefully paced. Low-impact exercises like walking, swimming, and stretching are generally recommended, but patients should stop before becoming fatigued.
9. What is a myasthenic crisis?
A medical emergency where muscle weakness becomes severe enough to compromise breathing, requiring immediate hospitalization and often mechanical ventilation.
10. How is MG diagnosed?
Through a combination of physical exam, blood tests for specific antibodies, nerve conduction studies (Repetitive Nerve Stimulation), and the Edrophonium (Tensilon) test.
11. What’s the difference between MG and ALS (Lou Gehrig’s Disease)?
MG is an autoimmune disorder that is treatable and does not affect life expectancy for most. ALS is a progressive, fatal neurodegenerative disease with no cure. Weakness in MG fluctuates; in ALS, it is progressive and permanent.
12. Can children get MG?
Yes, though it is rare. Juvenile Myasthenia Gravis is similar to the adult form. A transient form can also occur in newborns born to mothers with MG.
13. Why do my symptoms get worse in the afternoon or evening?
This is a hallmark of MG. Muscles become weaker with repeated use (fatigability) throughout the day and recover after periods of rest.
14. Are there any new treatments on the horizon?
Yes, research is ongoing into newer, more targeted biologic drugs (e.g., complement inhibitors like Eculizumab) that specifically block parts of the immune system involved in MG.
15. Does MG affect cognitive function or memory?
No, MG only affects the voluntary muscles. It does not damage the brain, nerves, or sensory functions.
16. Is there a special diet for MG?
No specific diet cures MG, but a balanced diet is important. If chewing or swallowing is difficult, a soft or pureed diet may be necessary.
17. Can I still work with MG?
Many people with MG continue to work successfully. Some may need accommodations, such as a flexible schedule or the ability to take rest breaks.
18. What is the role of the thymus gland in MG?
The thymus gland is believed to be involved in producing the faulty antibodies that attack the neuromuscular junction, which is why its removal (thymectomy) can be beneficial.
19. How long does it take to find the right treatment?
It can take months to over a year to find the optimal medication type and dosage that provides the best symptom control with the fewest side effects.
20. Where can I find support?
Organizations like the Myasthenia Gravis Foundation of America (MGFA) provide excellent resources, support groups, and the latest research information.
Conclusion
Myasthenia Gravis, once a “grave” diagnosis, is now a highly manageable chronic condition for the majority of patients. While its hallmark is weakness and fatigability of voluntary muscles, significant advances in understanding its autoimmune nature have led to a wide array of effective treatments. From medications and surgery to lifestyle adaptations, a multi-faceted approach allows individuals with MG to control their symptoms and lead active, fulfilling lives. Ongoing research continues to provide hope for even more targeted and effective therapies in the future.
Find Trusted Cardiac Hospitals
Compare heart hospitals by city and services — all in one place.
Explore Hospitals
This guide explains Myasthenia Gravis in a very clear and supportive way, especially how fluctuating muscle weakness can affect daily life and why early diagnosis and consistent treatment are so important for maintaining strength and independence. The connection you made between symptoms, medical care, and long-term management really helps patients and families understand that with proper monitoring and therapy, quality of life can be significantly improved. A very informative and reassuring resource for anyone trying to better understand this condition.