Introduction & Background of Takayasu’s Arteritis
Takayasu’s Arteritis (TAK), often called “pulseless disease,” is a rare and chronic form of vasculitis—a group of disorders that cause inflammation of the blood vessels. Specifically, Takayasu’s Arteritis is characterized by inflammation that damages the large arteries, with a predilection for the aorta (the main artery leaving the heart) and its primary branches, such as those supplying the head, arms, and kidneys.
The inflammation leads to thickening, scarring, and narrowing (stenosis) of the vessel walls, which can reduce blood flow to vital organs and limbs. In some cases, the vessel walls can weaken and bulge, forming an aneurysm. The disease most commonly affects young women, typically under the age of 40, and is more prevalent in Asia, though it occurs worldwide. The exact cause remains unknown, but it is classified as an autoimmune condition, where the body’s immune system mistakenly attacks its own arteries.
Causes of Takayasu’s Arteritis
The precise cause of Takayasu’s Arteritis is not well understood. However, it is widely regarded as an autoimmune disorder. The leading theories include:
- Autoimmune Response: The immune system mistakenly targets and attacks the body’s own arterial tissues, causing inflammation. The trigger for this misdirection is unknown.
- Genetic Predisposition: Certain genetic markers appear to be more common in people with Takayasu’s, suggesting a hereditary component that may make some individuals more susceptible.
- Infectious Triggers: Some researchers hypothesize that a prior bacterial or viral infection (e.g., tuberculosis) might trigger the autoimmune response in genetically predisposed individuals, but no specific pathogen has been proven to be the cause.
Indications of Takayasu’s Arteritis
“Iindications” often refer to the signs that lead a doctor to suspect the disease. These are typically discovered during examination and diagnostic testing:
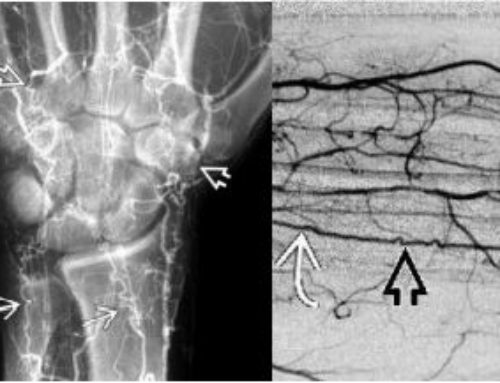
- Diminished or Absent Pulse: A key indicator, often in the wrist (radial pulse), leading to the name “pulseless disease.”
- Blood Pressure Difference: A significant difference ( > 10 mmHg) in blood pressure readings between arms.
- Bruits (Bru-ee): A whooshing sound heard with a stethoscope over narrowed arteries, particularly in the neck, abdomen, or under the collarbone.
- Imaging Findings: MRI, CT, or ultrasound scans showing thickening and inflammation of the aorta and its major branches.
Symptoms of Takayasu’s Arteritis
Symptoms are often divided into two phases:
1. Systemic Phase (Early, Pre-pulseless): Caused by generalized inflammation.
- Fatigue, malaise
- Unintended weight loss
- Mild fever
- Night sweats
- Muscle and joint pain
2. Occlusive Phase (Late, Pulseless): Caused by narrowed arteries and reduced blood flow.
- Arm or Leg: Claudication (pain, weakness, or cramping with use), coolness, numbness, weaker pulse in limbs.
- Brain: Dizziness, lightheadedness, fainting, headaches, visual disturbances, or strokes.
- Heart: Chest pain, shortness of breath (from high blood pressure, aortic valve disease, or coronary artery involvement).
- General: High blood pressure (often due to renal artery stenosis), anemia.
- Other: Chest pain, abdominal pain after eating (mesenteric ischemia).
Prevention Strategies of Takayasu’s Arteritis
There is no known way to prevent Takayasu’s Arteritis because the cause is unknown. However, the focus is on preventing complications and disease progression:
- Early Diagnosis and Treatment: Seeking medical attention for unexplained systemic symptoms can lead to earlier intervention.
- Medication Adherence: Strictly following prescribed immunosuppressive therapy to control inflammation and prevent further vessel damage.
- Regular Monitoring: Attending all follow-up appointments for blood pressure checks, blood tests, and imaging studies to catch new narrowings or aneurysms early.
- Healthy Lifestyle: Managing cardiovascular risk factors, such as maintaining a healthy weight, not smoking, and controlling blood pressure, is crucial to protect the heart and blood vessels.
Myths and Facts About Takayasu’s Arteritis
| Myth | Fact |
|---|---|
| It only affects women. | While it predominantly affects young women (90%), it can also occur in men and people of all ages. |
| It is contagious. | Takayasu’s is an autoimmune disease, not an infection. It cannot be spread from person to person. |
| It’s a form of cancer. | It is an inflammatory condition, not cancer. The treatments, however, often involve powerful drugs also used in cancer therapy. |
| If you feel fine, you can stop your medication. | The disease can be active even without obvious symptoms. Stopping medication without medical supervision can lead to silent progression and severe damage. |
| There is no treatment. | While there is no cure, effective treatments can control inflammation, manage symptoms, and prevent long-term complications. |
| Surgery is a cure. | Surgery fixes the structural damage (narrowing or aneurysm) but does not address the underlying inflammation. Medical therapy is still needed post-surgery. |
Treatments and Therapy
The goal of treatment is to suppress inflammation, control symptoms, and prevent permanent damage.
Medication-Based Treatments
- Corticosteroids (e.g., Prednisone): The first-line treatment to quickly reduce inflammation. Long-term use requires careful management due to side effects.
- Immunosuppressants (e.g., Methotrexate, Azathioprine, Mycophenolate): Used to maintain remission and allow for a reduction in steroid dosage (“steroid-sparing” agents).
- Biologics (e.g., Tocilizumab): Target specific parts of the immune system. Tocilizumab (an IL-6 receptor blocker) is now a key therapy for steroid-resistant or relapsing disease.
Surgical Treatments
Required when arterial damage causes critical narrowing or aneurysms.
- Bypass Grafting: Creating a new pathway for blood flow using a graft to bypass a blocked artery.
- Angioplasty and Stenting: A minimally invasive procedure to open a narrowed artery and place a stent to keep it open.
- Aortic Valve Replacement: If the aortic valve is damaged.
- Aneurysm Repair: To prevent the rupture of a weakened, bulging artery.
Physical Therapy and Rehabilitation
Helps improve muscle strength and endurance, reducing the symptoms of claudication and improving overall functional capacity.
Lifestyle and Behavioral Interventions
- Heart-Healthy Diet: Low in salt and saturated fat to help manage blood pressure and cholesterol.
- Smoking Cessation: Critical, as smoking severely damages blood vessels.
- Regular, Gentle Exercise: As tolerated, to improve circulation and cardiovascular health.
Alternative and Complementary Medicine
- Focus: These are supportive, not curative. Practices like yoga, tai chi, and meditation may help manage stress and improve well-being.
- Caution: Always discuss supplements with a doctor, as they can interact with medications.
Psychotherapy and Counseling
Living with a chronic illness is challenging. Counseling can help patients cope with anxiety, depression, body image issues, and the stress of managing a long-term condition.
Immunizations and Vaccines
Patients on immunosuppressants should receive recommended inactivated vaccines (e.g., flu shot, pneumonia vaccine) but should avoid live vaccines. This is a crucial part of preventive care.
Stem Cell Therapy
An area of active research for severe, treatment-resistant cases. It involves “resetting” the immune system, but it is not a standard treatment and carries significant risks.
Gene Therapy
Currently in the very early stages of basic science research. It is not a current treatment option for Takayasu’s Arteritis.
Top 20 FAQ with Answer on Takayasu’s Arteritis
1. Is Takayasu’s Arteritis fatal?
- With modern treatment, the prognosis is good. However, if untreated, complications like stroke, heart failure, or aneurysm rupture can be fatal.
2. What is the life expectancy for someone with Takayasu’s?
- Life expectancy is near normal with proper treatment and monitoring. The focus is on quality of life and managing complications.
3. Is Takayasu’s Arteritis hereditary?
- While not directly inherited, there may be a genetic predisposition that increases risk.
4. Can Takayasu’s go into remission?
- Yes, the goal of treatment is to induce and maintain remission, a state with no disease activity or symptoms.
5. Can I get pregnant if I have Takayasu’s?
- Yes, but it is considered a high-risk pregnancy. It requires careful planning and management by a team of specialists to ensure the disease is in remission and blood pressure is well-controlled.
6. What is the difference between Takayasu’s and Giant Cell Arteritis (GCA)?
- Both affect large arteries, but GCA typically affects older adults (over 50) and primarily targets the arteries in the head, especially the temples.
7. Why is my blood pressure different in each arm?
- This is a classic sign of Takayasu’s, caused by narrowing of the subclavian artery supplying one arm, reducing the pressure reading on that side.
8. Will I need surgery?
- Not everyone needs surgery. It is reserved for cases where critical narrowing or aneurysms develop and cause severe symptoms.
9. Are the medications used for Takayasu’s safe long-term?
- They require careful monitoring for side effects. The benefits of controlling the disease usually outweigh the risks, which your doctor will manage.
10. What kind of doctor treats Takayasu’s Arteritis?
- Usually a rheumatologist (autoimmune disease specialist), often working with a team including cardiologists and vascular surgeons.
11. Can children get Takayasu’s?
- Yes, though it is very rare in children.
12. Does diet affect Takayasu’s?
- No specific diet treats the inflammation, but a heart-healthy diet is vital to manage blood pressure and overall cardiovascular health.
13. Why am I always so tired?
- Fatigue is a very common symptom, stemming from both the active inflammation and the reduced blood flow to muscles and tissues.
14. Can the pulse come back after treatment?
- If the narrowing is not too severe, reducing inflammation can sometimes improve blood flow and make the pulse detectable again. However, fixed scar tissue will not resolve, and the pulse may remain absent.
15. How is it diagnosed?
- Through a combination of physical exam, blood tests (e.g., ESR, CRP for inflammation), and imaging like MRA, CTA, or ultrasound to visualize the arteries.
16. What triggers a flare-up?
- Triggers are not well-defined, but often include stopping medication or reducing the dose too quickly. Stress or infections can sometimes precede a flare.
17. Can I exercise with Takayasu’s?
- Yes, regular, moderate exercise is encouraged to improve circulation and heart health. Listen to your body and avoid overexertion that causes pain.
18. Is there a cure?
- Currently, there is no cure, but the disease can be effectively managed as a chronic condition.
19. What should I do if I suspect I have Takayasu’s?
- See your primary care doctor and describe your symptoms. Mention your specific concerns about Takayasu’s, and ask for a referral to a rheumatologist.
20. Where can I find support?
- Patient advocacy groups like the Vasculitis Foundation offer invaluable resources, educational materials, and connections to support communities.
Conclusion
Takayasu’s Arteritis is a rare but serious chronic condition that causes inflammation of the body’s large arteries. While its cause remains elusive and a cure is not yet available, significant advancements in diagnosis and treatment have dramatically improved outcomes. Through a combination of vigilant medical management, lifestyle adjustments, and, when necessary, surgical intervention, individuals with Takayasu’s can lead full and active lives. Ongoing research continues to shed light on the mechanisms of the disease, offering hope for even more effective and targeted therapies in the future.
Find Trusted Cardiac Hospitals
Compare heart hospitals by city and services — all in one place.
Explore Hospitals
This article offers a clear and compassionate explanation of Takayasu’s arteritis, helping readers understand how inflammation of the large arteries can lead to symptoms like reduced pulses, fatigue, and organ complications. The breakdown of typical signs, diagnostic approaches, and the importance of early detection makes the condition more accessible for patients and caregivers who may be encountering this rare disease for the first time. I also appreciate the practical discussion of treatment strategies and long-term management, which encourages informed conversations with healthcare professionals. Overall, it’s an informative and patient-centric resource that raises awareness and supports those navigating this complex condition.