Introduction & Background of Wilson’s Disease – Copper Accumulation in the Body
Wilson’s Disease is a rare, inherited genetic disorder that causes excessive accumulation of copper in the body. Normally, the liver filters excess copper and releases it into bile, a digestive fluid, which is then excreted from the body through the intestines. In individuals with Wilson’s Disease, this process is impaired due to a mutation in the ATP7B gene. This gene is responsible for producing a protein that transports copper into bile. When this protein is defective, copper builds up in the liver, and eventually spills into the bloodstream, depositing in other organs—particularly the brain, eyes, and kidneys. If left untreated, the copper toxicity can cause severe liver damage, neurological and psychiatric disorders, and is ultimately fatal.
Causes of Wilson’s Disease – Copper Accumulation in the Body
The sole cause of Wilson’s Disease is genetic.
- Autosomal Recessive Inheritance: A person must inherit two faulty copies of the ATP7B gene—one from each parent—to develop the disease.
- Carrier Status: Parents of an affected individual are typically carriers (they have one normal gene and one faulty gene). Carriers do not show symptoms of the disease but can pass the faulty gene to their children.
- The Genetic Defect: The mutation in the ATP7B gene disrupts the body’s ability to regulate copper, leading to its pathological retention.
Indications of Wilson’s Disease – Copper Accumulation in the Body
Indications are the clinical signs that lead a doctor to suspect and test for Wilson’s Disease. They often appear between the ages of 5 and 35 but can occur at any age.
- Unexplained liver disease in a child, teenager, or young adult.
- Neurological symptoms like tremor, slurred speech, or difficulty with motor skills without another clear cause.
- Psychiatric symptoms of sudden onset, such as depression, anxiety, or personality changes.
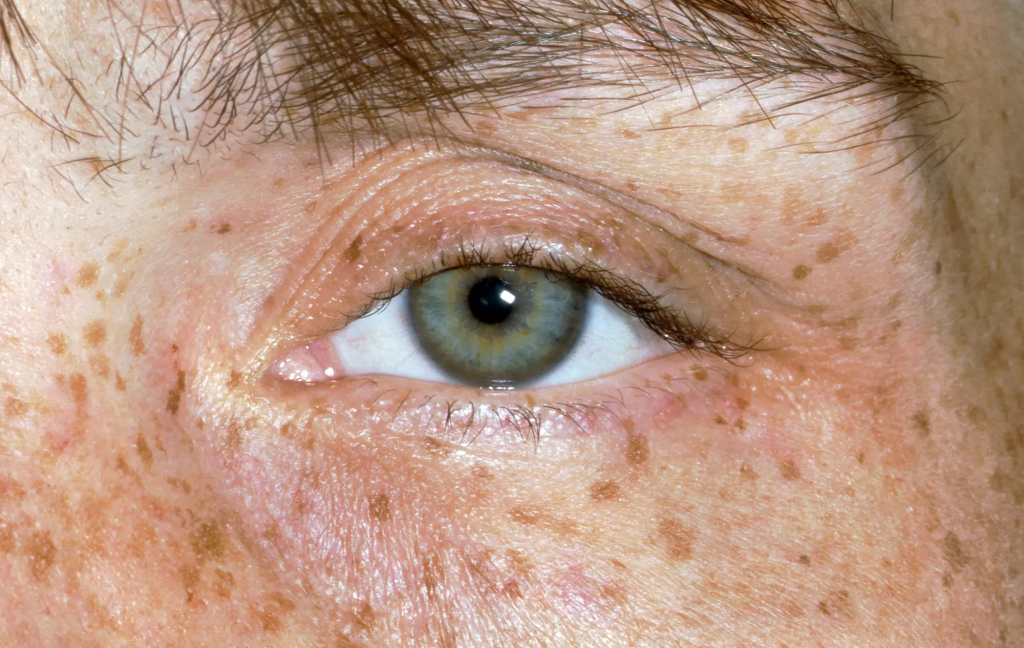
- The presence of Kayser-Fleischer (K-F) rings, a golden-brown discoloration in the cornea of the eye, visible through a slit-lamp examination.
- A family history of Wilson’s Disease.
Symptoms of Wilson’s Disease – Copper Accumulation in the Body
Symptoms are what the patient experiences and reports, and they are categorized by the organs affected.
Hepatic (Liver) Symptoms:
- Fatigue, weakness, and loss of appetite
- Jaundice (yellowing of the skin and eyes)
- Abdominal pain and swelling (ascites)
- Easy bruising and bleeding
- Spider angiomas (visible blood vessels on the skin)
Neurological Symptoms:
- Tremors, often beginning in the hands
- Muscle stiffness or dystonia (sustained muscle contractions causing abnormal postures)
- Slurred speech (dysarthria)
- Problems with walking, swallowing, and coordination
- Drooling
- Migraines
- Seizures (rare)
Psychiatric Symptoms:
- Depression, anxiety, and mood swings
- Personality changes
- Psychosis
- Impaired cognitive function
- Insomnia
Other Symptoms:
- Kayser-Fleischer rings (a key diagnostic sign).
- Sunflower cataracts in the lens of the eye.
- Kidney stones, arthritis, and, in women, menstrual irregularities and infertility.
Prevention Strategies of Wilson’s Disease – Copper Accumulation in the Body
As a genetic disease, Wilson’s itself cannot be prevented. However, its devastating symptoms and complications can be entirely prevented with early intervention.
- Genetic Counseling & Family Screening: If one child is diagnosed, all siblings must be tested. Genetic counseling can inform carriers of their risks when planning a family.
- Newborn Screening: While not yet widespread, research is ongoing to include Wilson’s Disease in newborn screening panels to allow for treatment before symptoms appear.
- Early Diagnosis and Lifelong Treatment: The most critical prevention strategy is diagnosing the condition early (often before symptoms arise) and adhering strictly to lifelong treatment to prevent copper buildup.
Myths and Facts About Wilson’s Disease – Copper Accumulation in the Body
| Myth | Fact |
|---|---|
| Wilson’s Disease is caused by a high-copper diet. | It is caused by a genetic defect. Diet only becomes a factor after diagnosis, where low-copper intake helps manage the condition. |
| Only children get Wilson’s Disease. | While often diagnosed in young people, it can first present in adults in their 40s or 50s. |
| It only affects the liver. | It is a multi-system disease that can severely impact the brain, eyes, kidneys, and other organs. |
| If you feel fine, you can stop your medication. | This is extremely dangerous. Treatment is lifelong. Stopping medication can cause rapid, acute liver failure that is often fatal. |
| It’s a common condition. | It is a rare disorder, affecting approximately 1 in 30,000 people worldwide. |
Treatments and Therapy
The goal of all treatment is to remove excess copper and prevent its reaccumulation.
Medication-Based Treatments
- Chelating Agents: These drugs bind to copper in the body and help remove it through urine.
- D-penicillamine: The first drug used, but has significant side effects.
- Trientine: Often better tolerated than D-penicillamine.
- Zinc Salts (e.g., Zinc Acetate): Zinc blocks the absorption of copper from the diet in the intestines and promotes the body’s natural excretion of copper in stool. It is often used for maintenance therapy or in presymptomatic patients.
Surgical Treatments
- Liver Transplant: This is reserved for cases of acute liver failure or advanced cirrhosis that does not respond to medication. A transplant cures the metabolic defect, as the new liver can regulate copper normally.
Physical Therapy and Rehabilitation
- Crucial for patients with neurological symptoms to improve muscle strength, coordination, balance, and speech (through speech therapy).
Lifestyle and Behavioral Interventions
- Diet: Avoiding copper-rich foods (liver, shellfish, mushrooms, nuts, chocolate, and some dried fruits) is recommended, especially in the first year of treatment.
- Alcohol Avoidance: Alcohol can worsen liver damage and is strictly prohibited.
- Water Check: Testing home well water for copper content is advised.
Alternative and Complementary Medicine
- No alternative therapy can replace copper-lowering medication. Some patients may use supplements like antioxidants under medical guidance, but these are complementary and not curative.
Psychotherapy and Counseling
- Essential for managing the psychological impact of a chronic illness, coping with psychiatric symptoms, and adhering to treatment plans.
Immunizations and Vaccines
- Patients with liver disease should receive all recommended vaccinations, especially against Hepatitis A and B, to prevent additional liver injury.
Stem Cell Therapy
- Currently experimental and not a standard treatment. Research is exploring if stem cells could regenerate healthy liver tissue.
Gene Therapy
- A promising area of future research aimed at correcting the defective ATP7B gene. It is not yet available for clinical use.
Top 20 FAQ with Answer on Wilson’s Disease – Copper Accumulation in the Body
1. Is Wilson’s Disease contagious?
No, it is an inherited genetic disorder and cannot be caught from another person.
2. At what age does it usually start?
Symptoms typically appear between ages 5 and 35, but diagnosis can occur in older adults.
3. Can Wilson’s Disease be cured?
There is no cure, but it is highly treatable. Lifelong medication can effectively manage the condition and allow for a normal life.
4. What is the life expectancy for someone with Wilson’s Disease?
With early diagnosis and strict, lifelong treatment, life expectancy is normal.
5. Is a liver transplant a cure?
Yes, a transplant replaces the defective liver and corrects the underlying copper metabolism problem. It is considered a cure for the disease.
6. Can I eat a normal diet?
After diagnosis, you must follow a low-copper diet, especially initially. Your doctor will provide a list of foods to avoid.
7. What happens if I miss a dose of my medication?
You should never miss a dose. Consistent medication is vital. If you do miss one, contact your doctor for advice. Do not double the next dose.
8. Can women with Wilson’s Disease have children?
Yes, with careful management. Treatment must continue throughout pregnancy under close medical supervision.
9. How is it diagnosed?
Through blood tests (ceruloplasmin, copper), 24-hour urine copper test, eye exam for K-F rings, and sometimes a liver biopsy.
10. What is a Kayser-Fleischer ring?
A golden-brown ring around the cornea of the eye caused by copper deposition. It is a key diagnostic sign.
11. Is it painful?
The disease itself is not typically described as painful, but symptoms like abdominal swelling and muscle cramps can cause discomfort.
12. Can the neurological damage be reversed?
With treatment, many neurological symptoms can improve or stabilize, and further damage is prevented. Some existing damage may be permanent.
13. Should my family get tested?
Yes, all first-degree relatives (siblings and parents) should be screened for the disease.
14. What is the difference between D-penicillamine and Trientine?
Both are chelators, but Trientine generally has a more favorable side-effect profile than D-penicillamine.
15. Can Wilson’s Disease cause mental illness?
Yes, it can present with serious psychiatric symptoms like depression, anxiety, and psychosis, which often improve with treatment.
16. How often do I need to see my doctor?
Regular follow-ups are essential, initially every few months, and then once or twice a year for stable patients.
17. Can I drink alcohol?
No. Alcohol can cause further damage to the liver and should be completely avoided.
18. Is it fatal?
If left undiagnosed and untreated, it is always fatal. With treatment, the prognosis is excellent.
19. What specialist treats Wilson’s Disease?
Patients are typically managed by a hepatologist (liver specialist) or a neurologist, often in a multidisciplinary team.
20. Why is it called Wilson’s Disease?
It is named after Dr. Samuel Alexander Kinnier Wilson, the British neurologist who first described the condition in 1912.
Conclusion
Wilson’s Disease is a serious but manageable genetic condition. The key to a positive outcome lies in awareness and early diagnosis. While the disease can affect multiple organs and present with a wide array of symptoms, the availability of effective medications and, in severe cases, liver transplantation, means that most patients can lead full and productive lives. Ongoing medical supervision, strict adherence to treatment, and family screening are the cornerstones of successful long-term management. Continued research into gene therapy holds promise for even more advanced treatments in the future.
Find Trusted Cardiac Hospitals
Compare heart hospitals by city and services — all in one place.
Explore Hospitals
This article explains Wilson’s Disease in a very clear and compassionate way, especially how it connects copper buildup with liver, neurological, and behavioral symptoms. I appreciated the strong focus on early diagnosis, proper treatment, and lifelong monitoring, which helps readers understand how timely care can significantly improve outcomes. Informative, patient-friendly, and very helpful for spreading awareness about this important metabolic disorder