Introduction & Background of Goodpasture Syndrome
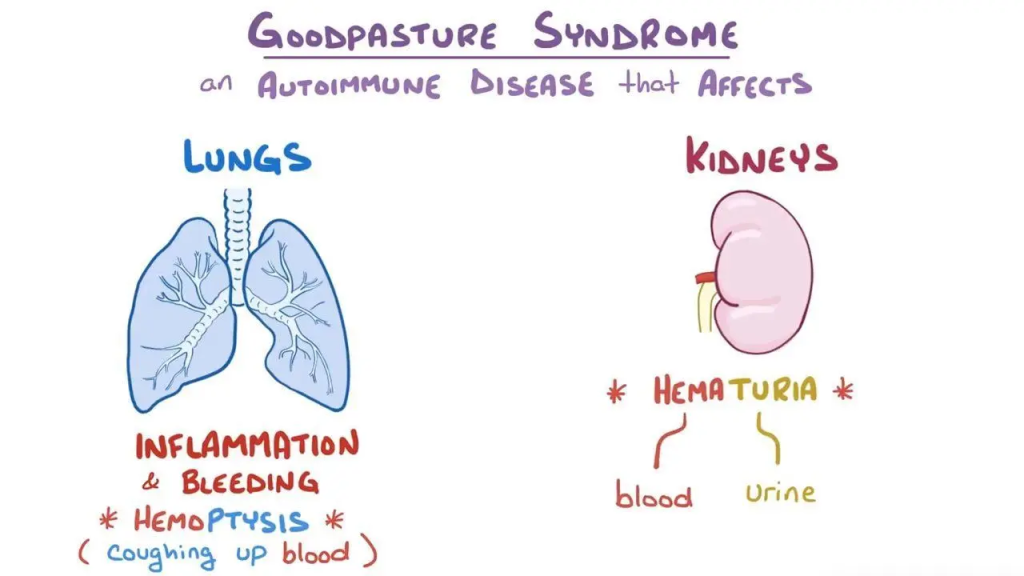
Goodpasture Syndrome (GPS), also known as Anti-Glomerular Basement Membrane (Anti-GBM) disease, is a rare and life-threatening autoimmune disorder. In this condition, the body’s immune system mistakenly produces antibodies that attack two critical organs: the lungs and the kidneys.
These antibodies specifically target proteins in the basement membranes of the alveoli (air sacs in the lungs) and the glomeruli (filtering units in the kidneys). The primary target is the alpha-3 chain of type IV collagen, a key structural component of these membranes. This attack leads to inflammation and damage, causing the lungs to bleed (pulmonary hemorrhage) and the kidneys to fail rapidly (rapidly progressive glomerulonephritis). Early diagnosis and aggressive treatment are crucial to prevent permanent organ damage and save lives.
Causes of Goodpasture Syndrome
The exact cause of Goodpasture Syndrome is not fully understood, but it is believed to result from a combination of genetic predisposition and environmental triggers.
- Autoimmune Mechanism: The core problem is a malfunction of the immune system. The body produces autoantibodies against the Goodpasture antigen (the alpha-3 chain of type IV collagen) in the basement membranes.
- Genetic Predisposition: Individuals with certain genetic markers, particularly HLA-DR15, are at a higher risk of developing the disease.
- Environmental Triggers: In genetically susceptible people, the following factors may trigger the onset:
- Inhalants: Exposure to hydrocarbon solvents, cigarette smoke, or certain metallic dusts.
- Infections: Viral respiratory infections (e.g., influenza) or bacterial infections.
- Drugs: Certain medications like alemtuzumab or cocaine (contaminated with levamisole).
- Physical Factors: Lung injury from trauma or procedures.
Indications of Goodpasture Syndrome
“Indications” often refer to the signs that lead a doctor to suspect the disease. Key indications include:
- Hemoptysis: Coughing up blood (from a pink-tinged sputum to frank blood) is the most common lung symptom and a major red flag.
- Rapidly Worsening Kidney Function: Blood and protein in the urine (detected by dipstick), rising serum creatinine levels, and a rapid decline in the glomerular filtration rate (GFR).
- Constitutional Symptoms: Fatigue, weakness, nausea, loss of appetite, and pallor (pale skin) due to anemia from lung bleeding and kidney failure.
- A Positive Anti-GBM Antibody Test: This is the definitive laboratory indication.
Symptoms of Goodpasture Syndrome
Symptoms can appear suddenly and worsen quickly.
- Lung-related Symptoms:
- Coughing up blood (hemoptysis)
- Shortness of breath (dyspnea)
- Dry cough
- Chest pain
- Respiratory failure (in severe cases)
- Kidney-related Symptoms:
- Blood in the urine (hematuria) – may be visible (cola-colored) or microscopic
- Protein in the urine (proteinuria) – often causing foamy urine
- Swelling (edema) in the legs, ankles, and around the eyes
- High blood pressure
- Reduced urine output
- General Symptoms:
- Severe fatigue and weakness
- Nausea and vomiting
- Pale skin
- Fever (less common)
Prevention Strategies of Goodpasture Syndrome
Since the exact cause is unknown and involves genetic and unpredictable environmental factors, there is no known way to prevent Goodpasture Syndrome. However, for individuals diagnosed or at high genetic risk, the following may be considered:
- Avoid Known Triggers: Refrain from smoking and avoid exposure to hydrocarbon solvents, paints, and metallic dusts.
- Prompt Infection Control: Seek early treatment for respiratory infections.
- Awareness and Early Detection: Individuals with a family history or known genetic risk should be aware of the symptoms and seek immediate medical attention if they develop.
Myths and Facts About Goodpasture Syndrome
| Myth | Fact |
|---|---|
| Goodpasture Syndrome is a type of cancer. | It is an autoimmune disease, not cancer. The immune system attacks the body’s own tissues. |
| It is contagious. | It is not contagious. You cannot catch it from someone who has it. |
| Only older people get it. | It can occur at any age, but it has a bimodal distribution, peaking in young men (20s-30s) and older adults (60s-70s). |
| If you have it, you will definitely need lifelong dialysis. | Early and aggressive treatment can often preserve kidney function. While some patients do progress to end-stage renal disease, others recover significant kidney function. |
| It only affects the lungs and kidneys. | While the lungs and kidneys are the primary targets, the autoimmune process is systemic and can cause general symptoms like severe fatigue and anemia. |
Treatments and Therapy
Treatment aims to stop the production of harmful antibodies, remove existing antibodies from the blood, and control inflammation.
Medication-Based Treatments
- Corticosteroids: High-dose intravenous (IV) methylprednisolone is used initially to quickly suppress widespread inflammation, especially in the lungs.
- Immunosuppressive Drugs: Drugs like cyclophosphamide or rituximab are used to halt the production of new anti-GBM antibodies by suppressing the immune system.
- Plasma Exchange (Plasmapheresis): This is a cornerstone of treatment. The patient’s blood plasma, which contains the harmful antibodies, is removed and replaced with donor plasma or albumin. This rapidly reduces the level of attacking antibodies in the circulation.
Surgical Treatments
- Kidney Transplant: For patients who suffer permanent, end-stage kidney failure, a transplant is an option. It is usually performed only after the anti-GBM antibodies have been undetectable for several months to prevent recurrence in the new kidney.
Physical Therapy and Rehabilitation
- Used during recovery to rebuild muscle strength and physical endurance, especially if the patient was critically ill or bedridden.
Lifestyle and Behavioral Interventions
- Dietary Changes: A renal diet, low in salt, potassium, and protein, is often necessary to manage kidney disease and high blood pressure.
- Smoking Cessation: Absolutely critical to prevent further lung damage.
- Infection Prevention: Due to immunosuppressive therapy, patients must be vigilant about hand hygiene and avoiding sick contacts.
Alternative and Complementary Medicine
- No alternative therapies can treat GPS itself. However, practices like meditation, yoga, and acupuncture may help some patients manage the stress and side effects of treatment, but only under medical guidance.
Psychotherapy and Counseling
- A diagnosis of a rare, life-threatening illness is profoundly stressful. Counseling can help patients and families cope with anxiety, depression, and the major life changes the disease imposes.
Immunizations and Vaccines
- Patients on immunosuppressants should generally avoid live vaccines. It is crucial to stay up-to-date with recommended inactivated vaccines (e.g., flu shot, pneumococcal vaccine) to prevent infections, ideally before starting immunosuppression.
Stem Cell Therapy
- This is not a standard treatment for Goodpasture Syndrome and is considered highly experimental. Research is ongoing in the broader field of autoimmune diseases.
Gene Therapy
- Gene therapy is not currently a treatment option for Goodpasture Syndrome and remains in the realm of future scientific research.
Top 20 FAQ with Answers on Goodpasture Syndrome
1. Is Goodpasture Syndrome fatal?
It can be if not treated promptly. With modern treatment, the survival rate is over 80%, but kidney damage may be permanent.
2. What is the life expectancy for someone with Goodpasture Syndrome?
With successful treatment, life expectancy can be normal, though it depends on the extent of organ damage at diagnosis. Many patients live long lives, some with ongoing kidney disease management.
3. Is Goodpasture Syndrome hereditary?
There is a genetic predisposition (linked to HLA-DR15), but it is not directly inherited in a simple Mendelian pattern. Having a family member with it slightly increases risk, but it’s still very rare.
4. How is it diagnosed?
Through blood tests (to detect anti-GBM antibodies), urine tests (for blood and protein), and a kidney biopsy (which shows a characteristic linear pattern of antibody deposition).
5. What’s the difference between Goodpasture Syndrome and Anti-GBM disease?
They are often used interchangeably. Strictly speaking, “Goodpasture Syndrome” refers to the clinical presentation of both lung hemorrhage and kidney disease. “Anti-GBM disease” is the broader term for the condition, which can sometimes only affect the kidneys.
6. Can the lung and kidney damage be reversed?
Lung damage often heals well once bleeding is controlled. Kidney damage is more variable; if treated early, function can be recovered, but advanced damage is often irreversible.
7. Will I need dialysis?
It depends on the severity of kidney injury at presentation. Many patients require temporary dialysis during the acute phase. Some may recover enough function to stop, while others with severe damage will need lifelong dialysis.
8. Can I get a kidney transplant?
Yes, it is a successful option for those with end-stage kidney failure. Doctors typically wait until anti-GBM antibodies are undetectable for 6-12 months to minimize the risk of recurrence.
9. What are the side effects of treatment?
Immunosuppressants increase the risk of infections. Cyclophosphamide can cause hair loss, bladder irritation, and infertility. Long-term steroids can lead to weight gain, diabetes, and bone thinning.
10. Can Goodpasture Syndrome come back?
The risk of relapse is very low (<5%) compared to other autoimmune diseases, especially if the initial treatment successfully eliminates the antibodies.
11. Who is most at risk?
It most commonly affects two groups: young men in their 20s-30s and older adults (men and women) in their 60s-70s.
12. Can children get it?
Yes, but it is extremely rare in children.
13. What should I do if I start coughing up blood?
This is a medical emergency. Go to the nearest emergency department immediately.
14. Is there a special diet for Goodpasture Syndrome?
You will likely need to follow a kidney-friendly diet, tailored by a renal dietitian based on your specific kidney function and electrolyte levels.
15. Can I still work and exercise?
After the acute phase and during recovery, most patients can return to work and light exercise. Your medical team will provide guidance based on your lung and kidney function.
16. Does this affect pregnancy?
Pregnancy can be high-risk for both mother and baby in someone with a history of GPS. It requires careful planning and management by a high-risk obstetric team and a nephrologist.
17. Why is it called Goodpasture Syndrome?
It is named after Dr. Ernest Goodpasture, who first described a patient with the condition in 1919 while investigating the influenza pandemic.
18. Are there support groups for this condition?
Yes, organizations like the National Kidney Foundation (USA) and the Rare Diseases Clinical Research Network can provide resources and connect patients.
19. How long does treatment last?
The intensive phase (plasmapheresis and high-dose immunosuppression) typically lasts for several weeks. Oral immunosuppressants are usually continued for several more months until antibodies remain undetectable.
20. What is the most important factor for a good outcome?
Early diagnosis and immediate initiation of treatment are the most critical factors in saving lives and preserving kidney function.
Conclusion
Goodpasture Syndrome is a formidable autoimmune disease that launches a simultaneous attack on the lungs and kidneys. While its rarity and rapid progression make it a medical emergency, significant advances in treatment—primarily plasma exchange and immunosuppressive therapy—have transformed it from a universally fatal condition to one with a high survival rate. The journey for patients often involves managing the long-term consequences, particularly chronic kidney disease. Ongoing research continues to improve our understanding of its triggers and mechanisms, offering hope for even more effective and targeted therapies in the future.
Find Trusted Cardiac Hospitals
Compare heart hospitals by city and services — all in one place.
Explore Hospitals
This guide explains Goodpasture Syndrome in a very clear and reassuring way, especially how lung and kidney symptoms are connected and why early diagnosis is critical to prevent serious complications. The way you described warning signs, treatment options, and long-term care really helps patients and families understand the importance of timely medical support and regular monitoring. A very informative and supportive resource for anyone trying to better understand this rare but serious autoimmune condition.