Introduction & Background of Anti-NMDA Receptor Encephalitis
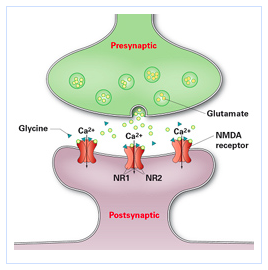
Anti-NMDA Receptor Encephalitis is a severe form of autoimmune encephalitis (brain inflammation) where the body’s own immune system mistakenly produces antibodies that attack the NMDA (N-methyl-D-aspartate) receptors in the brain. These receptors are crucial for synaptic transmission, memory, learning, and behavior.
First identified in 2007 by Dr. Josep Dalmau and his team, it has become one of the most common and well-known types of autoimmune encephalitis. It primarily affects young adults and children, with a significant female predominance, but it can occur at any age and in any gender. The condition gained public attention through the book and film Brain on Fire, which chronicled a patient’s experience.
Causes of Anti-NMDA Receptor Encephalitis
The primary cause is the production of autoantibodies that target the GluN1 subunit of the NMDA receptor. The trigger for this autoimmune response is not always clear but is often linked to:
- Teratomas (Ovarian Tumors): The most well-established association, particularly in young women. The teratoma contains neural tissue that expresses NMDA receptors, triggering the immune system to produce antibodies that cross-react with the brain’s receptors.
- Other Tumors: Less commonly, other tumors like testicular teratomas in men or other neoplasms can be a trigger.
- Viral Infections: Herpes simplex virus (HSV) encephalitis is a known trigger. After recovering from the initial viral infection, some patients develop autoimmune encephalitis as a “post-infectious” phenomenon.
- Unknown Triggers (Idiopathic): In a substantial number of cases (up to 50%), no tumor or clear triggering infection is identified. It is believed other, yet undiscovered, immune system triggers are at play.
Indications of Anti-NMDA Receptor Encephalitis
“Indications” refer to the signs that should lead a clinician to suspect this diagnosis. It is often misdiagnosed as a psychiatric illness initially.
- Atypical Psychiatric Symptoms: Sudden, severe psychosis, agitation, or catatonia in a previously healthy young person.
- Neurological Symptoms Following a Flu-Like Prodrome: The development of seizures, memory loss, or movement disorders after a minor illness.
- A Combination of Symptoms: The hallmark is the rapid progression through a characteristic series of symptoms: flu-like illness -> psychiatric features -> neurological deficits (seizures, movement disorders) -> autonomic instability (fluctuating heart rate, blood pressure) -> decreased consciousness.
- Poor Response to Standard Treatments: Lack of response to antipsychotic medications or standard epilepsy treatments.
Symptoms of Anti-NMDA Receptor Encephalitis
Symptoms typically progress through stages over weeks or months:
- Prodromal Phase (Days to Weeks): Headaches, low-grade fever, fatigue—resembling a mild viral illness.
- Psychiatric Phase: Anxiety, insomnia, agitation, paranoia, hallucinations (visual and auditory), manic behavior, and psychosis.
- Neurological Phase:
- Seizures: Various types, including generalized tonic-clonic.
- Movement Disorders: Repetitive, involuntary movements like lip-smacking, grimacing, or rhythmic motions of the limbs or trunk.
- Memory Deficits: Profound short-term memory loss (amnesia).
- Speech Problems: Mutism (inability to speak), echolalia (repeating others’ words), or pressured speech.
- Cognitive Decline: Disorientation and confusion.
- Autonomic Dysfunction: Fluctuations in heart rate, blood pressure, temperature, and breathing rate. This can be life-threatening.
- Decreased Consciousness: Progressing to a catatonic state, unresponsiveness, or coma.
Prevention Strategies of Anti-NMDA Receptor Encephalitis
There is no known way to prevent the initial onset of the disease, as the autoimmune response is unpredictable. However, prevention focuses on:
- Early Tumor Removal: For patients with a known teratoma, surgical removal is both a treatment and a preventive measure against severe relapse.
- Prompt Treatment of Relapses: For patients with a known history of the disease, early intervention at the first sign of relapse can prevent a full-blown episode.
- Vigilance Post-Viral Infection: Close monitoring of patients recovering from viral encephalitis (like HSV) for the emergence of autoimmune symptoms.
Myths and Facts About Anti-NMDA Receptor Encephalitis
| Myth | Fact |
|---|---|
| It’s a rare form of schizophrenia or bipolar disorder. | It is a physical disease of the brain, not a primary psychiatric disorder. However, it causes psychiatric symptoms. |
| It only affects young women. | While most common in young women, it can affect men, children, and the elderly. |
| If you have it, you definitely have a tumor. | Only about 50-60% of female patients have an associated tumor (usually ovarian teratoma). The percentage is lower in other groups. |
| It’s always fatal. | With modern treatments, approximately 75-80% of patients have a good functional recovery, though it can be a long process. Mortality is around 5-10%. |
| Recovery means all symptoms disappear completely. | Many patients recover significantly, but some may have long-term cognitive deficits, fatigue, or emotional challenges. |
Treatments and Therapy
Treatment is multi-faceted and aims to remove the source of antibodies, suppress the immune attack, and manage symptoms.
Medication-Based Treatments
- First-Line Immunotherapy:
- Corticosteroids: (e.g., Methylprednisolone) to reduce inflammation broadly.
- Intravenous Immunoglobulin (IVIG): A pool of antibodies from donors that can modulate the immune system.
- Plasmapheresis (PLEX): “Plasma exchange” to physically remove harmful antibodies from the blood.
- Second-Line Immunotherapy: Used if there is no response to first-line treatments.
- Rituximab: A monoclonal antibody that depletes B-cells (the cells that make antibodies).
- Cyclophosphamide: A stronger chemotherapy agent that suppresses the immune system.
Surgical Treatments
- Tumor Removal: If a teratoma or other tumor is found, its surgical resection is critical and often leads to dramatic improvement.
Physical Therapy and Rehabilitation
- Essential for rebuilding strength, coordination, and motor skills lost during the prolonged illness and hospitalization.
Lifestyle and Behavioral Interventions
- Structured Routine: Helps with cognitive and memory retraining.
- Cognitive Rest: Avoiding overstimulation during early recovery.
- Healthy Diet and Sleep Hygiene: Supports overall brain recovery.
Alternative and Complementary Medicine
- Mindfulness and Meditation: Can help manage anxiety and stress during recovery.
- Acupuncture: Some patients find it helpful for pain and residual neurological symptoms. Note: These should complement, not replace, standard medical care.
Psychotherapy and Counseling
- Cognitive Rehabilitation Therapy: Specifically targets memory, attention, and executive function deficits.
- Psychotherapy: Helps patients and families process the traumatic experience of the illness, manage mood disorders, and adjust to any lasting changes.
Immunizations and Vaccines
- There is no vaccine to prevent this disease. During treatment with immunosuppressants, live vaccines are contraindicated.
Stem Cell Therapy
- Not a standard treatment. It is considered only in the most severe, refractory cases that have not responded to all other immunotherapies and is largely experimental.
Gene Therapy
- Currently, there is no role for gene therapy in the treatment of Anti-NMDA Receptor Encephalitis. Research is focused on the immune system, not the genes.
Top 20 FAQ with Answer on Anti-NMDA Receptor Encephalitis
1. What is Anti-NMDA Receptor Encephalitis?
It is an autoimmune disease where the immune system attacks NMDA receptors in the brain, leading to severe inflammation and a wide range of neurological and psychiatric symptoms.
2. Who gets it?
It can affect anyone, but it is most common in young women and children.
3. Is it contagious?
No, it is an autoimmune disorder and cannot be passed from person to person.
4. What are the first signs?
Often, flu-like symptoms followed by sudden, severe psychiatric problems like anxiety, paranoia, or hallucinations.
5. How is it diagnosed?
Through a combination of clinical symptoms, brain MRI, EEG, and most definitively, by detecting anti-NMDA receptor antibodies in the blood or cerebrospinal fluid (CSF) via a lumbar puncture (spinal tap).
6. Is it fatal?
It can be, especially if untreated, but with early diagnosis and aggressive treatment, the majority of patients survive.
7. What is the recovery rate?
About 75-80% of patients have a significant or full recovery, though this can take months or even years.
8. Can it come back (relapse)?
Yes, the relapse rate is approximately 10-15%, usually within the first two years.
9. What causes it?
It is often triggered by a tumor (like an ovarian teratoma) or, less commonly, by an infection. In many cases, the trigger is unknown.
10. How is it treated?
Treatment involves immunotherapy (steroids, IVIG, plasmapheresis, rituximab) and, if present, removal of a tumor.
11. How long does treatment last?
The acute phase can last weeks to months. Immunotherapy may be continued for months or years to prevent relapse.
12. What are the long-term effects?
Some patients may have persistent issues with memory, concentration, fatigue, or mood disorders.
13. Is it a mental illness?
No, it is a neurological disease that causes psychiatric symptoms. The root cause is physical, not psychological.
14. Can children get it?
Yes, it is a leading cause of autoimmune encephalitis in children.
15. What is the connection to the movie Brain on Fire?
The movie is based on the true story of a New York Post reporter, Susannah Cahalan, who survived the disease, raising massive public awareness.
16. Are you ever “cured”?
Many patients achieve full recovery, but some require long-term management. The goal is to achieve remission and prevent relapses.
17. What should I do if I suspect someone has it?
Seek immediate medical attention at a hospital with a neurology department. Emphasize the sudden onset of symptoms.
18. What is the role of family during recovery?
Family support is crucial. They are often the best advocates for the patient and play a vital role in rehabilitation and emotional support.
19. Can you work or go to school after recovery?
Many people return to work or school, but often require a phased return and accommodations due to cognitive fatigue.
20. Where can I find support?
Organizations like the Autoimmune Encephalitis Alliance and the Siegel Rare Neuroimmune Association provide resources, support networks, and information for patients and families.
Conclusion
Anti-NMDA Receptor Encephalitis is a serious but treatable disease. Over the past decade, awareness and understanding have grown dramatically, leading to faster diagnoses and better outcomes. While the journey to recovery can be long and challenging, the majority of patients can regain a significant quality of life. Continued research is vital to improving treatments, understanding triggers, and ultimately finding ways to prevent this devastating condition. For patients and families, early recognition, expert medical care, and a strong support network are the cornerstones of overcoming this illness.
Find Trusted Cardiac Hospitals
Compare heart hospitals by city and services — all in one place.
Explore Hospitals
This article offers a clear and compassionate explanation of anti‑NMDA receptor encephalitis, making a complex autoimmune brain disorder easier to understand for both patients and caregivers. The way it describes how the immune system attacks NMDA receptors and leads to symptoms like psychiatric changes, seizures, and movement problems helps demystify this serious condition. I also appreciate the focus on early recognition, diagnostic approaches, and modern treatment strategies, which are crucial for improving outcomes. Overall, it’s an informative and patient‑centered resource that raises awareness and supports informed discussions with healthcare professionals.